Robin Roberts: 'GMA' Anchor Gets Bone Marrow Transplant to Treat MDS
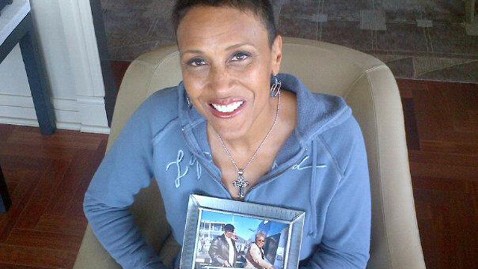
Facebook/RobinRoberts
"Good Morning America" co-anchor Robin Roberts underwent a bone marrow transplant Thursday to treat MDS, a bone marrow disorder that affects blood cells production.
The transplant was a five-minute procedure in which the donor cells from Robin's sister, Sally-Ann, were injected into Robin's system through a syringe.
"Nobody can believe it," Dr. Gail Roboz, the New York-Presbyterian Hospital/Weill Cornell Medical Center oncologist who is treating Robin, said today on "GMA" of the short procedure.
"People have in their mind all kinds of images of what can happen in a transplant but it's still an incredibly powerful moment," she said. "Inside of that syringe are millions and millions of stem cells that are now circulating around and trying to find their home and start growing which is what we're going to be looking for over the next couple of weeks."
As she underwent the transplant Robin was surrounded by her siblings and other loved ones, including "World News" anchor Diane Sawyer and "GMA"'s weather anchor, Sam Champion.
Click HERE to read the latest message from Robin
"It was an emotional, scary and yet exhilarating moment, one that I'll never forget," Champion said.
Robin faced the procedure with grace, strength and humor. For 10 days prior to the transplant, she endured rigorous chemotherapy treatments to prepare her system to accept her sister's cells.
Prior to the procedure, the Rev. A.R. Bernard prayed. Then, slowly and steadily, Dr. Sergio Giralt injected the millions of donor stem cells. After the procedure, Robin and her family and friends broke out in one of her favorite songs, "Ain't No Mountain High Enough."
"I will now wait and anxiously watch and see what happens," Robin said after the procedure. "In the next seven to 10 days my counts will continue to go up and we'll be on to phase three, which will be get out of here. Get out of here. Go home. It's a journey."
Click HERE to Follow Robin's Journey
So what's next?
"I got a good email this morning," Roboz said. "This morning she [Robin] sounds energized and she wants to be out of bed and the end of the email was "I want to go home" with an exclamation point."
Robin, according to Roboz, will lack energy in the next few days. She may have persistent indigestion and heartburn, and won't have much of an appetite. She will have chills, and may have a fever.
"We have to roll with the punches over the next few days because, don't forget, her systems are down and Sally-Ann's aren't up yet so we're in that in between zone of watching very carefully," she said. "We are wanting every day to be a good day but we are ready for some bumps in the road."
Doctors will treat Robin with intravenous fluids, electrolyte replacement and anti-viral, anti-bacterial and anti-fungal medications, Roboz said. Though she'll be monitored daily, doctors won't expect to see significant signs of recovery for about 10 days. They will closely watch her for signs of infection.
Since her immune system was destroyed to make way for the new cells, she would be unable resist infection in her own.
"We actually check blood sometimes several times a day," Roboz said. "You can start seeing normal blood cells recover and usually what I tell people is when you get three days in a row of the white blood cells coming up, then you're starting to get excited that the graf is taking hold. The stem cells are talking hold and maybe we're going to start getting to he finish line and getting out of the hospital."
In two weeks or so, Robin should begin to feel better. Once the transplanted cells start to do their job, there is generally significant improvement in how patients feel, Roboz said. The primary goal of the transplant is to get Robin's system to correctly produce white blood cells and platelets.
To find out more about bone marrow donation and sign up for a registration kit from the Be the Match Registry, click HERE.
Even though Robin's sister was a perfect match, Robin's system will still try to attack the donor cells. Doctors will work to prevent any symptoms of graft vs. host disease - a rejection of the bone marrow transplant.
Robin's time in the hospital will be determined by how well her body adapts to the transplant. The markers for recovery typically come at 30 days and then 100 days post-transplant.
Send 'GMA' Your #TeamRobin Photo
Your Questions Answered
Roboz has answered questions the "GMA" staff and fans had about Robin's treatment, procedure and recovery process. Read her edited answers below.
The day a patient receives a bone marrow transplant is often called "Day Zero." What are the benchmarks in Robin's progress from there?
Days 0 - 30: The first 30 days are when the new cells are setting up shop and getting ready to regenerate. So many of my patients ask me, when the catheter is placed in her chest for the transplant, 'How do these cells know where to go? How do they find the bone marrow?' These cells have homing signals to help them find where they need to go and start growing and creating an environment for themselves.
…
"Early recovery" is when the bone marrow is taking hold, and blood is being created normally.
[Until her donated cells engraft and] she starts making blood cells and platelets on her own, she's completely dependent on platelet and blood transfusions. It's about filling in for what your system can't do. It can't fight infections. The medications have to fight everything that's out there. You can't make cells or platelets, so you'll have transfusions. You can't eat, so we give you something to keep you nourished.
….
This is a tough time in the treatment. There are mouth sores, weight loss, diarrhea, food doesn't taste good, there's hair loss.
What will her hospital set-up be like during this period?
The team is there the whole time, monitoring how you're feeling, what your experiencing, constantly. It's not the "intensive care unit" but it's intensive care.
What will you be looking for and monitoring in the first 30 days?
We need to get through that period of wiped-out blood counts. We'll start to see white blood cells, red blood cells and platelets growing on their own. That's the evidence that the graph is working. That's when we breathe our initial sigh of relief. She'll need fewer transfusions, fewer medications, she'll be getting out of the hospital [after 30 days]. At that point, she'll still be on significant meds to regulate her immune system, but she'll be recovering at that point.
Talk about Days 30 to 100.
Starting at that 30 Day mark, she'll have bone marrow evaluations to see that it's growing normally.
In the days that follow - until the 100 day benchmark - we're seeing problems getting solved. She'll get off the meds, she won't feel as tired or as gross as you do when you're on so many pills. She'll start liking to eat again. She'll have to remind herself what she likes to do. You're separated from all that stuff for so long, you have to slowly reintroduce yourself to what you used to do.
Will she want visitors?
Probably not every day. It's a day to day thing. Well-wishers have to understand that the patient drives what's best for them. Sometimes it's best to let someone sleep.
When does she go home?
If all goes well, Robin will go home after 30 days.
When she goes home she won't be feeling like herself, but we hope she'll be able to do some exercises, read and focus. It's important not to put a time stamp on anything. People are variable. Especially the way people are micromanaged in this process. You can't be worried if you're slower than others.
When will she feel like herself again?
Transplant is an individual experience. …We can't tell you how and when someone will feel better. Some people say they didn't feel 100% for a year. Others are ready to go back out much earlier.
What happens after the 100-Day Mark?
We have to watch patients super-closely for 100 days. We don't trust anything for the first 100 days. After that, we're happy. With cancer patients, we use five years as a benchmark to a cure. When someone has had a marrow transplant, we'll be watching her for life, to see if she's having symptoms.
How will you monitor when Robin will be able to come back to work?
We'll need to see high blood counts that don't require transfusions. She must be totally off antibiotics. Feeling sharp. There's an extra high bar for her because she has a harder job than most. She needs to have her system all up and running - marrow, immune system, nutrition - everything that was wiped out in chemotherapy has to be restored.