Liberian Community in Texas Raises Concerns About Dallas Ebola Patient's Treatment
Thomas Eric Duncan was visiting Texas from Liberia.
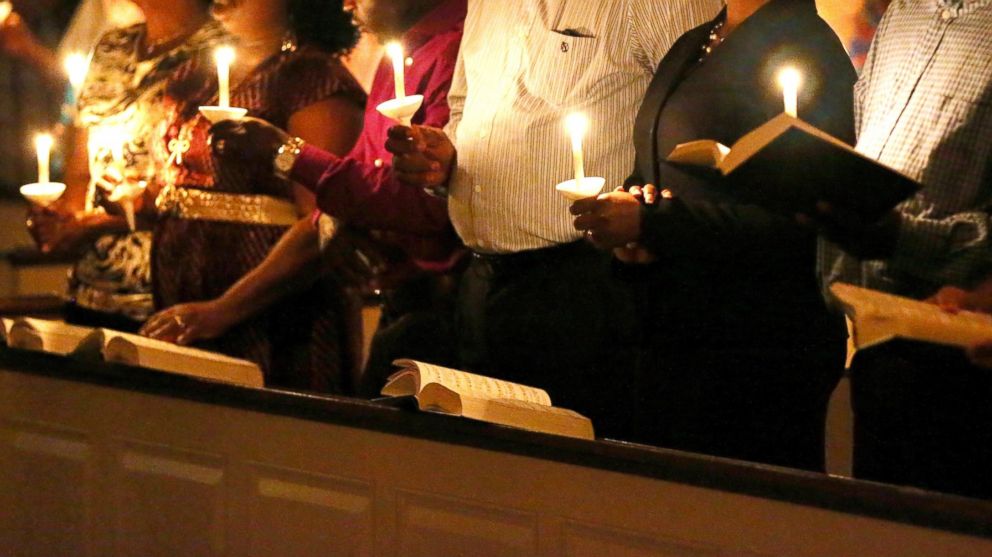
— -- The death of Thomas Eric Duncan, a Liberian man who was the first patient in the U.S. to die of Ebola, is stirring debate in the Dallas Liberian community about whether there has been a difference in the quality of treatment between American and African patients with Ebola at U.S. hospitals.
Stanley Gaye, president of the Liberia Community Association in Dallas, said people have contacted him about concerns that Duncan was treated differently “because he was African and not only that, he was Liberian.”
Texas Health Presbyterian Hospital explained today in detail how they cared for Duncan, including assigning 50 people to help with Duncan's care and securing an entire intensive care unit for Duncan.
However, Gaye told ABC News that one of the biggest concerns expressed by the Liberian community was that Duncan was allowed to leave that hospital on Sept. 25 even though he had early Ebola symptoms and had told a nurse there that he had recently traveled from West Africa.
Hospital officials initially said that there was a lapse in the record keeping system that allowed Duncan to leave even though he met criteria from the U.S. Centers for Disease Control and Prevention indicating he should be quarantined for possible Ebola infection. But they later said the system was functioning properly and have yet to give a further reason for the error.
In today's statement, the hospital denied Duncan had received substandard care during his first visit to the emergency room.
"Our care team provided Mr. Duncan with the same high level of attention and care that would be given any patient, regardless of nationality or ability to pay for care," read the statement, which clarified Duncan had a four-hour evaluation and numerous tests.
Three days later, on Sept. 28, Duncan was taken back to the hospital in an ambulance and put into an isolation ward at the hospital, health officials said.
Liberian community members have voiced concern that by not being admitted to the hospital immediately, the illness had time to make Duncan sicker and that “he was not properly taken care of,” Gaye said.
Duncan died from the Ebola virus on Wednesday, more than a week after being admitted to Texas Presbyterian Hospital. The day before his death, hospital officials said he was on a respirator and being given kidney dialysis.
He was also being given the experimental drug brincidofovir. Another Ebola patient, an American journalist being treated in Nebraska, has also started the same medication, health officials said.
Texas Health Presbyterian Hospital officials revealed new details today about Duncan's death and explained he had asked not to receive certain extraordinary measures, including chest compressions and defibrillation.
"In spite of the intensive care he was receiving, his heart stopped," the hospital said in its statement.
The hospital also adamantly defended its treatment of Duncan and explained why he had not received some of the same medications other Ebola patients had been given. Duncan's family told reporters on Wednesday that Duncan had received "unfair" treatment compared to other patients who had been cared for in the U.S.
“No one has died of Ebola in the U.S. before. This is the first time,” Weeks told ABC News.
Weeks said the family asked doctors at Texas Health Presbyterian Hospital why Duncan was not moved to Emory University Medical Center, where two missionaries were treated for Ebola earlier this year. Weeks said doctors told the family they had everything necessary to treat Duncan in Dallas.
The CDC has not recommended that Ebola patients be transferred to a specialized isolation facility like the one at Emory University.
Weeks also said doctors told the family Duncan was not given any donated plasma, called convalescent serum, from former Ebola patients. The hospital stated today that Duncan's blood type was not compatible with convalescent serum donors.
The hospital also affirmed that Duncan was not given ZMapp, a serum used on two U.S. healthcare workers, because the supply had been exhausted.
At least one expert said this information is crucial to rebuilding trust between nervous community members and medical institutions.
Art Caplan, a medical ethicist and director for Division of Medical Ethics at the New York University Langone Medical Center, said just the appearance of a hospital or medical institution treating patients differently can have severe negative consequences for public health during an epidemic.
Caplan said if people don’t trust health authorities then they might not seek help when they’re sick and inadvertently infect others.




