Nelson Mandela's Illness Puts Spotlight on Palliative Care
Palliative care offers relief from symptoms of serious illness.
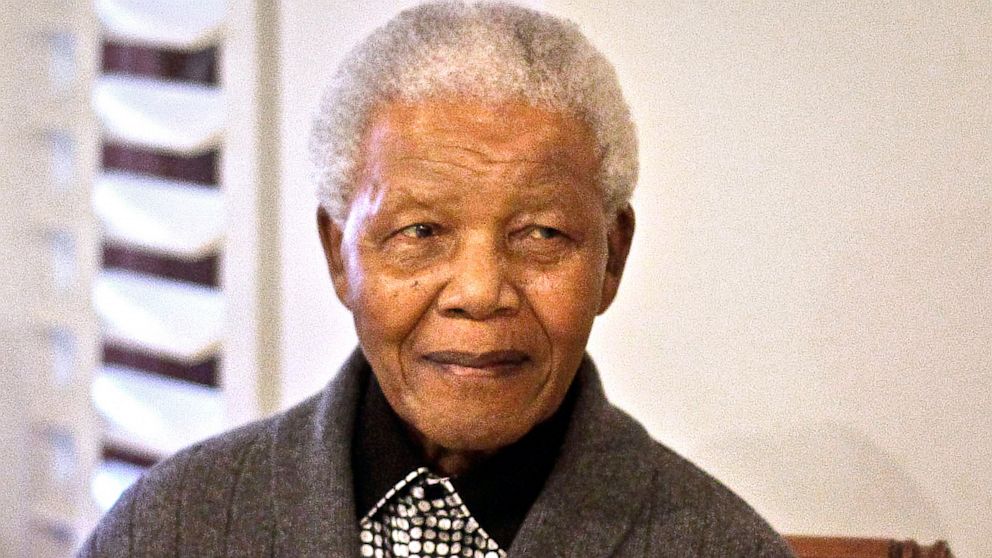
July 16, 2013— -- Ailing human rights icon Nelson Mandela's ill health and repeated hospital stays have put the spotlight on palliative care, a growing branch of medicine that provides seriously ill patients with relief from the symptoms, pain and the stress of sickness.
Palliative Care Tweet Chat Today at 1 p.m. ET
"Mandela is clearly an important public figure and his high-profile case helps raise awareness of palliative care," said Dr. Sean Morrison, director of palliative care at Mt. Sinai Medical Center in New York City.
Palliative care specialists, including doctors, nurses, social workers and other health care providers, work together to improve quality of life for patients and their families, Morrison said. Most palliative care physicians are internists or practice family medicine with an additional subspecialty and board certification in palliative medicine.
With approximately 90 million Americans living with a serious and life-threatening illness, according to the Center to Advance Palliative Care in New York City, medical experts say there is a pressing need for palliative services and programs. Dr. Diane Meier, director of the CAPC, estimates that at least six million chronically ill people in this country could benefit from palliative treatment.
"Illness doesn't just happen to the person who is sick, it happens to everyone around them too," she said. "Palliative care improves the lives of patients and anyone who loves and cares for them."
She pointed to a 2010 New England Journal of Medicine paper that found patients who receive early palliative care experienced less depression, improved quality of life and survived 2.7 months longer than patients who didn't receive the same care.
Early Palliative Care Cuts Time in the ICU
There is also some evidence that palliative care lowers medical care costs. For example, one recent study showed a $7,000 savings per hospital admission for patients receiving palliative care compared with those not receiving it. And another study showed that moving patients from the intensive care unit at New York City's Montefiore Medical Center to an acute palliative care unit within the hospital reduced the cost for hospital room and board by more than half, with additional savings on charges for ventilators and pharmacy costs.
"Because we can anticipate and treat unnecessary symptoms, there is a lot less reliance on acute medical care," Meier said. "This is better and less expensive for the patient and for the medical system, as a whole."
Although approximately 1,500 hospitals in the U.S. now offer access to palliative care, twice the number that offered such services just six years ago, Morrison said the average patient isn't familiar with the specialty and, even if they are, they don't know where it's offered or when to ask for it.
Palliative Care Aids Recovery of Some Lung Cancer Patients
"The appropriate time to seek out palliative care is at the time of diagnosis of any serious illness," he said. "It should be provided at the same time as all other treatment."
Dick Woodruff, the vice president of federal relations for the American Cancer Society Cancer Action Network, said even people who do know about palliative care tend to associate it with hospice, a service offered to patients who are likely facing death within a few months. But asking for a palliative care consultation doesn't mean giving up on a cure, as hospice does.




