Detroit hospitals 'getting crushed' as Michigan coronavirus cases surge
An alternate care facility is being built inside Detroit's TCF Center to help.
With rapidly increasing cases of the novel coronavirus in Michigan beginning to overwhelm the hospital system, one Detroit doctor says he's "not sure any level of preparedness would have been enough" to respond to the pandemic.
"I think it's fair to say that Detroit is getting crushed right now. … We were watching China and trying to anticipate how this would play out," Dr. Nick Gilpin, medical director for infection prevention at Beaumont Health, told ABC News. "But under the circumstances, this has been so fast and heavy."
On Thursday, there were 10,791 people in Michigan who had tested positive for the novel coronavirus, and 417 have died. The state reported its first two cases on March 10.
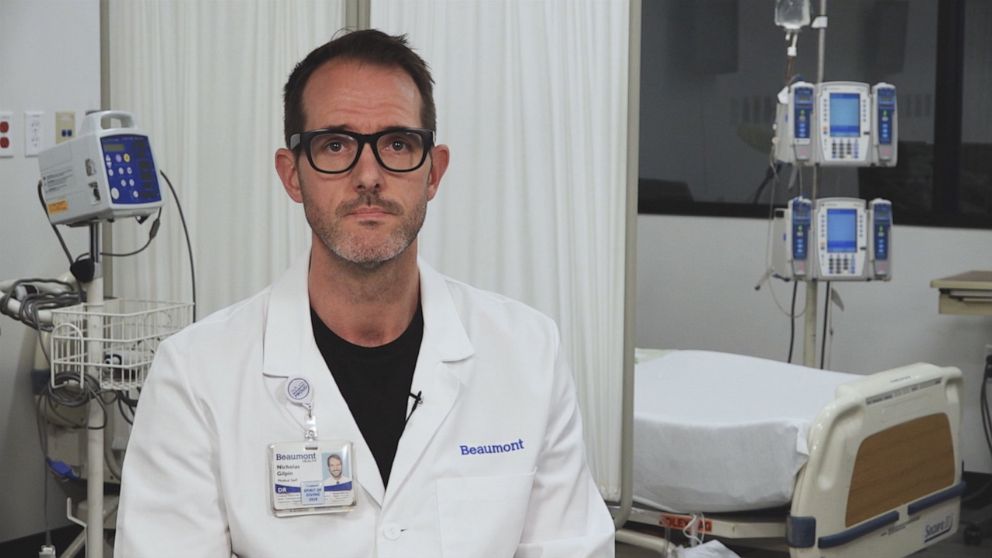
A high concentration of those cases have been in the southeastern part of the state, in Detroit, Wayne, Macomb and Oakland counties. Gilpin, who said he represents the Beaumont system's hospitals in Wayne and Oakland, speculated that it's Detroit's high density and medically underserved population that has made them vulnerable to COVID-19.
"I think the Detroit area, as many of us who have practiced here for years know, [has] greater per capita incidents of obesity [and] medical conditions like diabetes and lung disease built up over years," he said.
With his hospitals 70% to 80% occupied by COVID-19 patients, Gilpin said the challenges they face change every day.
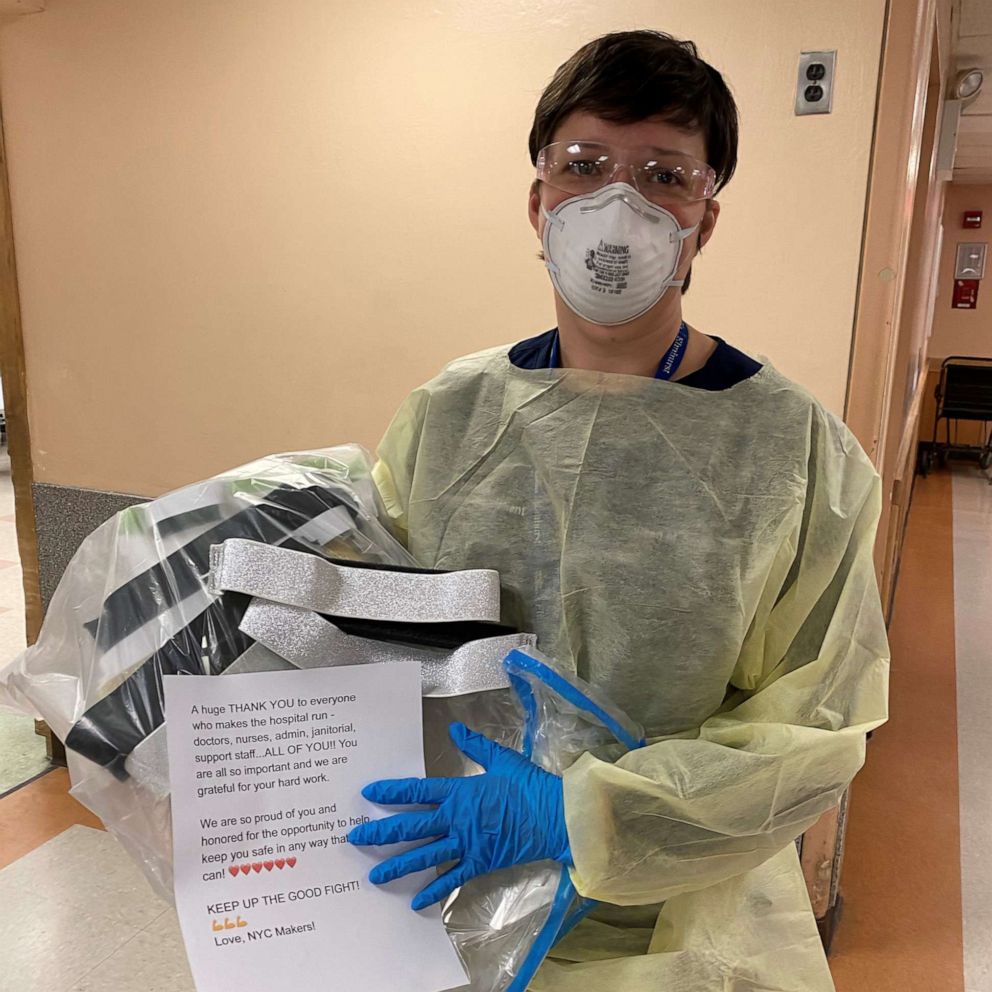
"A week ago, my challenges were all about supply," Gilpin said, pointing specifically to personal protective equipment, which he said they've resorted to reusing in hopes of easing the strain.
"Now, my real challenge is staffing," he added. "I worry a lot about my staff. It frankly keeps me up at night. … Are they sick? Are they psychologically and emotionally burdened from what they are seeing each day that it's difficult to keep coming to work?
"The mantra has become: 'We have to protect the staff, we have to preserve the PPE at all costs.' And that is obviously in addition to making sure we're doing the right thing for the patients."
Gilpin echoed sentiments from Mary Macdonald, an emergency room nurse in Michigan whose Instagram video explaining issues she's seen in hospitals, went viral last week. In the video, Macdonald said she had been called to work on her day off for an overnight shift during which she put someone on the hospital's last available ventilator. She said the N95 mask she's been using is "signed out for the entire year" when they're meant to be single-use.
"We are completely out of resources," Macdonald said. "There are no masks, there are no gowns. They're running low on gloves. … We cannot stay safe and we cannot care for all these people that are coming in."
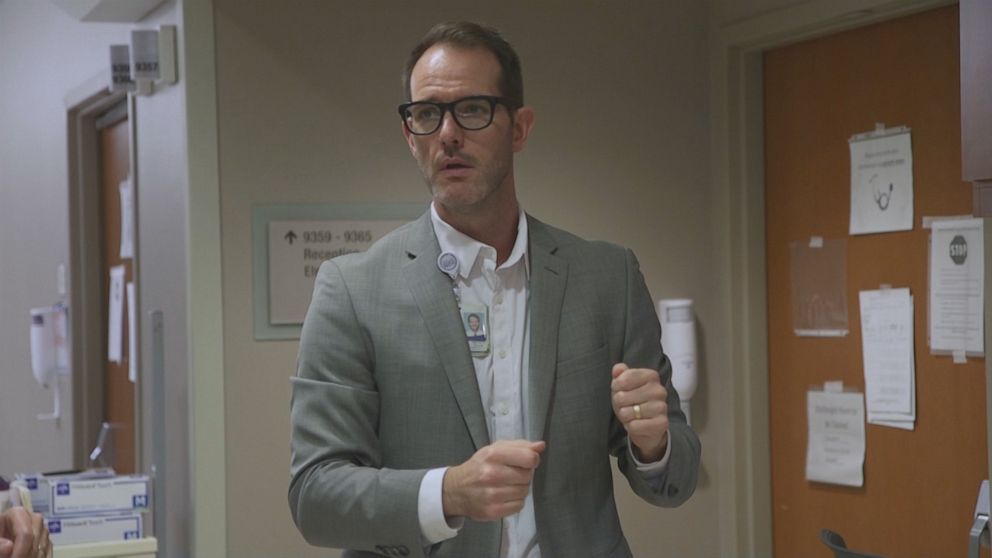
Staffing shortages, Gilpin said, will likely become the biggest challenge over the next few weeks if the surge in cases carries on. He offered one strategy to remediate this potential issue, which he called "load balancing."
"We have a significant amount of COVID concentrated in metro Detroit," he said. "But if you drive 30 minutes away, you see considerably less COVID in that part of the state. So we could take some of our existing patients and potentially move them to other facilities for care, or perhaps we could take some ventilators or resources from areas less affected and fairly balance the load between us."

He said Beaumont Health is already doing this "on a micro level" among its campuses and with neighboring health systems, but that it needs to be done statewide.
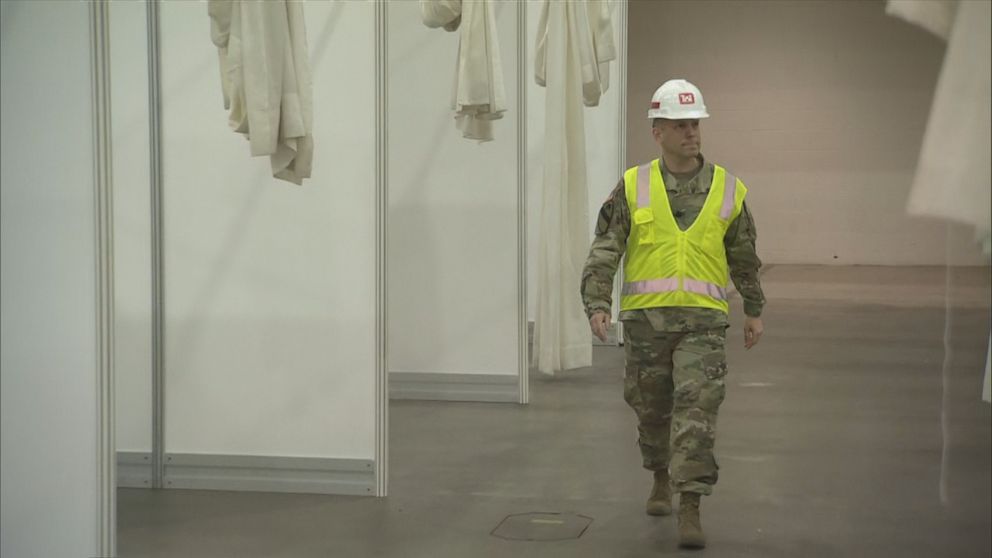
At the direction of the Federal Emergency Management Agency, the U.S. Army Corps of Engineers has been brought to Detroit to ease the burden on hospitals by building an alternate care facility in the TCF Center in downtown Detroit.
Lt. Col. Greg Turner, who has been leading the effort, said the facility would hold up to 1,000 COVID-19 patients and that certain precautions would be built in to ensure the virus doesn't spread, such as gearing the ventilation system up for negative pressure and specialized areas for dressing and undressing PPE.
Like Gilpin, Turner said that staffing has been a concern among the medical experts with which he's been consulting.

"The state of Michigan acknowledged that there is a staffing shortfall," Turner said, noting that the facility's capacity had been planned with this shortage in mind. "Regardless of how much staff ... there is only a certain number [of patients] that they can really effectively manage."
The team has been working hard to get the facility construction done by April 9 or earlier, said Turner, who hopes it'll be operational by mid-April.
Turner said that although he's been through many crises, none have been like this.
"This reminds me of my time spent in New Orleans [in] 2005 responding to Hurricane Katrina, when I was ... helping out down there providing distribution and keeping that place safe," Turner said. "The corps itself responded to Hurricane Katrina, Superstorm Sandy -- a lot of other large-scale disasters. Now, this is different, cause it's nationwide and it's something that we're not used to. But we're ready for this."
ABC News' Neil Giardino, Jake Lefferman and Kristopher Rios contributed to this report.
This report was featured in the Wednesday, April 8, 2020, episode of “Start Here,” ABC News’ daily news podcast.
"Start Here" offers a straightforward look at the day's top stories in 20 minutes. Listen for free every weekday on Apple Podcasts, Google Podcasts, Spotify, the ABC News app or wherever you get your podcasts.