3-D printed ovaries help mice get pregnant, show promise for fertility treatments
3-D printing is one of the new frontiers for replacing tissues and organs.
— -- In the era of regenerative medicine, which seeks to develop replacement tissues and organs in the lab for the millions of people in need, 3-D printing is a new frontier. The technology has already been harnessed to create everything from human skin to bone and heart tissue to cartilage for use during surgery and transplants.
Ovaries may be the next 3-D printed organ, holding promise for some of the estimated 6.1 million women who struggle with infertility in the U.S., according to the CDC.
Yesterday, a mouse study published in Nature Communications described a first crucial step to pave the way for this technology: successfully using 3-D printing to create mouse ovaries that, when implanted into mice, resulted in live births.
The "bioprosthetic" was conceived with female cancer survivors in mind, who often lose their ovarian function due to intensive chemotherapy treatments, which can cause absence of puberty, early menopause and infertility.
If further studies show the technology works in humans, it could also offer options for women who have a condition called primary ovarian insufficiency, where ovarian function diminishes before the age of 40.
"A successful human bioprosthetic could have a wide range of applications," said Dr. Monica Loranda, the lead author of the paper and researcher at Northwestern University. She said the women who may be helped include those who have reproductive development disorders, had cancer as children or who had rheumatological disease.

Current options to restore fertility and hormone function in cancer survivors include in-vitro fertilization and ovarian transplants. But these options are limited and often do not provide long-term solutions.
Researchers aimed to develop a whole organ replacement as a potential long-term solution to restore normal hormonal function and fertility. The answer: a 3-D printed bioprosthetic ovary, engineered from a combination of biomaterials and ovarian cells. One huge advantage to pursuing this strategy is that organs can be grown using cells from the same patient, bypassing any risk of rejection via the body's immune system once transplanted.
Loranda and her colleagues initially tried to test the theory by using portions of cow ovaries, stripped down to their base components, something called a ‘decellularized matrix’ that they seeded with mouse ovarian cells. However, the cow ovary matrix couldn't support the growth of the cells, Loranda said.
After that first attempt, they looked for another way to create the "bioprosthetic." and decided to use a 3-D printed ovary. The challenge was to design a model that organically supported ovarian follicles, which contains cells responsible for maturing the eggs released during a menstrual cycle, as well as cells that release hormones like estrogen and progesterone.
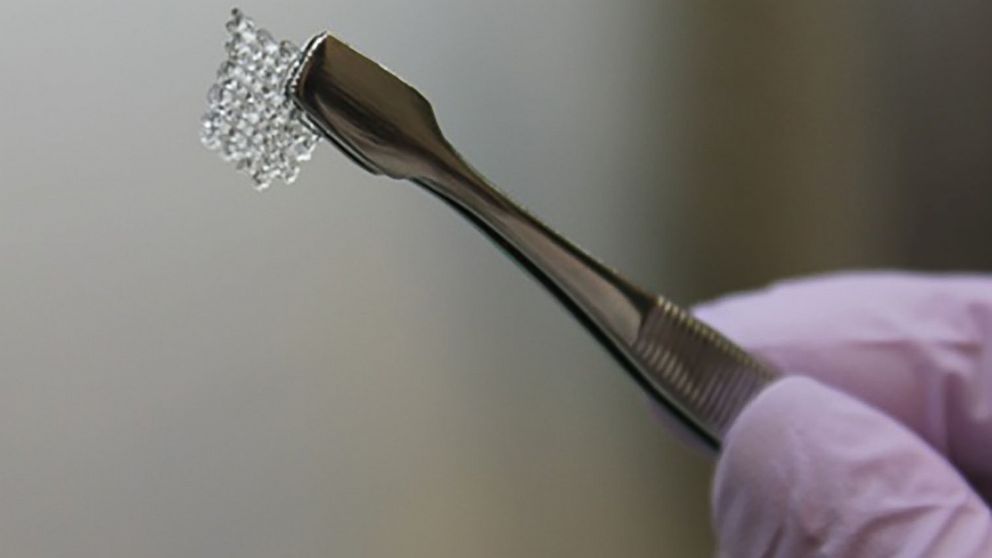
Researchers created a "scaffold" printed a collagen, gel-like porous bioprosthetic that mimicked the structure of a mouse ovary, optimized for nutrient and blood flow, which are essential to the survival and function of the organ. The scaffold was then seeded with the ovarian follicles. Finally, they implanted the 3-D printed ovaries into female mice that previously had their ovaries removed.
Once placed inside the mice, the bioprosthetic ovary flourished. Normal egg maturation was observed, with hormones production in response ovulation and menstruation cues. Even more promising, the mice were able to become pregnant and give birth to pups.
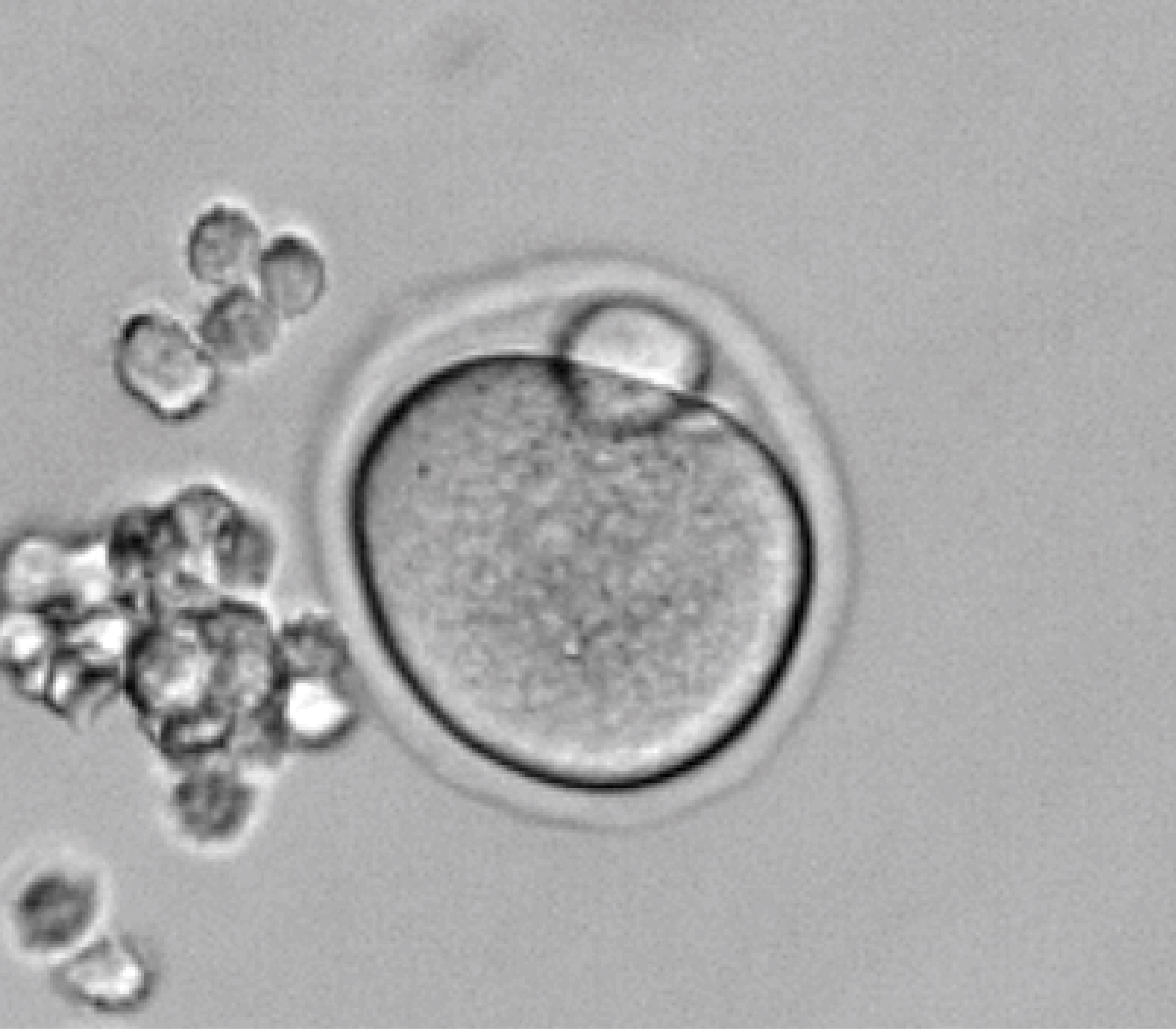
Researchers left oviducts (the equivalent of fallopian tubes in humans) intact to test whether mice could normally conceive offspring after natural mating, comparing them against mice implanted with "sham scaffolds" that did not have the ovary cells.
Three mothers with bioprosthetic ovaries fostered healthy litters of pups, while those with sham scaffolds did not. The 3-D printed ovaries supported implantation of the egg and produced the hormones required for pregnancy, and even lactation, after birth.
Researchers found the initial results to be promising, but much more experimentation will be necessary before the technique can be fully adapted to humans.
Next, they will need to test the findings on larger animals and work to adapt the process, eventually, to mimic human ovaries which will take continuing studies over several years.
Nonetheless, Laronda is excited by the potential prospects of this technology.
"I really hope that in the future it would provide an additional option to patients who don't have very many, restoring natural hormonal function and fertility."
Priya Raja is a Medical Fellow in the ABC News Medical Unit as a part of the Stanford - ABC News Global Health and Media Fellowship. She is also a rising third year medical student at The University of Texas Southwestern Medical Center.




