In coronavirus response, we only get 2 strikes: OPINION
How the U.S. might come back, carefully but purposefully, in wake of pandemic.
The month of social distancing that lies ahead should not be simply dedicated to slowing the spread. It must be viewed as a precious opportunity to mount a massive mobilization of people, equipment, ingenuity and test capacity to enable a responsible return.
When the novel coronavirus first appeared, the experts told us how to slow its spread, and the president bought us an extra month to prepare by stopping travel from China. Unfortunately, things went wrong and we didn’t use that time effectively. That was strike one.
The same experts have told us how to responsibly return to normal without causing a second wave. Let’s take their advice and not waste this precious second chance. In this game, we only get two strikes.
This will require selfless leadership, vision and hard work. We have to look beyond our headlights, plan our course and speed, and do the hard work that goes into a long journey that will continue all summer.
Let’s be clear about what went wrong on our first swing at coronavirus. The social distancing strategy was developed in the mid-2000s by a team of distinguished experts led by Dr. Rajeev Venkayya. It was groundbreaking work commissioned by President George W. Bush, and its principles remain sound. It envisioned people and communities taking early and aggressive steps to slow the spread of illness in a targeted, layered, community-based, not country-wide, fashion. Its authors presumed we would be able to identify the sick and lock down specific cities and states with clarity and precision.
Two humbling problems hampered the implementation of that strategy.

First, we could not easily identify the levels of human-to-human transmission that were growing invisibly across our vast country. Public health officials wanted highly reliable results from diagnostic tests designed to detect very early infections before antibodies are developed in the patient.
These are advanced and complicated tests, and there were massive shortfalls of needed capacity at a critical time. Thus, the coronavirus spread undiagnosed. Without the precision diagnostic testing data they desperately wanted, public health officials felt hard pressed to justify the aggressive, targeted interventions envisioned by the strategy. To compound the problem, once the supply of tests began to slowly improve, the demand for testing started to increase exponentially. We have been chasing that moving target ever since.
Second, public health officials showed reticence to act without the highly reliable precision of the diagnostic tests we lacked, even as warning signs of the coming crisis began to demonstrate the need for early action, most strikingly in China and later in Italy. Nevertheless, we waited. By mid- to late-February many in the public health community wanted to give up hope in perfect diagnostic data and shift to an approach that would've been good enough to expand the health surveillance net with clinical diagnostics.
Tune into ABC at 1 p.m. ET and ABC News Live at 4 p.m. ET every weekday for special coverage of the novel coronavirus with the full ABC News team, including the latest news, context and analysis.
Public health officials refer to this as syndromic surveillance. The idea was to deem patients that presented with upper respiratory symptoms and fever, testing negative for seasonal influenza, as presumptive positives for the purpose of directing intervention efforts, hospital supplies, and economic assistance with greater fidelity and confidence.
We might never know what difference a broader approach would've made, but the indicators were there. Diagnostic tests weren't needed to see the problem in New York City. The chart below, with data that is reported weekly, shows syndromic surveillance. You can see the impact of coronavirus in red. Illness Surveillance Network data on influenza-like illness showed a restart of flu-like illness after the seasonal flu spike had already ended. The evidence was clear by week 10, March 1 to 7.
By mid-March, there was no choice but to issue nationwide social distancing guidelines. Two weeks later, we still had no choice but to extend for another 30 days. That does not mean the virus will be defeated by April 30. Far from it.
If we want to step out of this 45-day national separation without causing a second wave of outbreak and economic loss, we must do it thoughtfully, and we better get started.
The current U.S. case count has topped 300,000 with more than 8,000 deaths.
But at some point, the horses are going to want to come out of the barn. Households, businesses, schools, and churches will need criteria, at the local level, for easing back into business, and the necessary administrative and engineering controls that need to be put in place once that next phase begins.
The experts tell us we must pursue de-escalation of social distancing at different times in different places aided by extensive testing, aggressive contact tracing, isolation and quarantine. This is no easy task.
The massive mobilization of equipment, test capacity, and people required to achieve a state-by-state, county-by-county risk weighted approach cannot start soon enough. To do it right will be the challenge of our lifetimes, and it will involve virtual armies of volunteers and experts, hopefully aided by technology and testing, and maybe even techniques we have developed in special forces warfare -- like rapid responses to new intelligence. As former Navy SEAL Chris Fussell wrote in The Atlantic, "This war is being fought by governors, mayors, and hospitals, and they need a network that links them directly to one another, and moves as fast as the virus they are working to defeat."
This virus spreads directly during respiration and person-to-person contact and it spreads indirectly through contact with objects or materials that carry infection, such as clothes, utensils, and furniture. We can handle indirect transmission with cleanliness. To limit direct transmission, however, will require detective work.
On May 1, the virus will still be among us, living invisibly on surfaces and in people, like a minefield. On that day, we will not want to run blindly out of our homes into that minefield, lest we detonate a second wave of outbreak. There will be three kinds of people starting on May 1, and our job will be to sort them out, carefully and respectfully. There will be the susceptible, the infectious, and the already recovered.
Most of us will be susceptible. We will not have been infected and will not have immunities. We will be dry tinder that could easily reignite.

Some of us will be infectious, whether we know it or not. To determine who is infectious, we need tests, and lots of them.
The remainder of us will have been infected and recovered, and therefore most certainly immune to reinfection. To identify the recovered, we need two things, an accurate list of diagnostic test results -- for those who experienced symptoms and got tested -- and a blood test to detect antibodies in people that were infected and never knew it.
This all sounds good. But, as National Institute of Allergy and Infectious Disease Director Dr. Anthony Fauci cautioned, we must "examine the feasibility" of what we want to do. In other words, let’s get real.
Good communicators in a crisis give people relevant information they can use to make decisions. The information should have value to the people, not to the institution providing it. Good leaders set objectives and help people understand what is coming. What’s coming is hard work and a long, tedious summer.
Some places will need to maintain or even increase, not just relax, social distancing in May. The U.S. is a big country and a community-based approach is appropriate. However, we have to be careful not to be overly rigid in defining communities. Some counties and even states are linked daily by commuting realities, for example. Others are barely linked at all.
To unwind in a careful, community-based fashion will require a significant surveillance capability and a common, uniform standard. In other words, a lot more tests and an agreement on who gets tested and why. Otherwise, comparisons will be based on uneven and unreliable risk measurements and the allocation of resources will be baseless. We must work together and introduce some discipline into the system.
The objective number of tests needed to identify and clear a statistically meaningful number of infectious people from the virus minefield remains unclear, and a common, responsible screening standard has not been established.
We should be wary of an approach that simply accepts the number of available tests and backs into the health surveillance we can achieve, rather than the surveillance we actually need to clear enough mines. To maximize our chances, it will soon become appropriate to test the otherwise young and healthy with mild symptoms, and not the most intractable cases. We will have to change to focus to those who are mildly ill or not sick at all, and away from the very sick.

The goal is to isolate the infectious in controlled medical facilities. Voluntary isolation and voluntary quarantine of those with whom confirmed patients have had contact is a leaky proposition.
It took four months for the world to get to 250,000 cases. It took one week to go from 250,000 cases to 500,000 cases. We are now over one million and climbing. The need to trace contacts and quickly isolate and separate the infectious from the susceptible will require organized effort, people, discipline, and perhaps smartphone apps and other ingenuity.
All of it will require time and effort to mobilize. We have less than four weeks to make decisions, decide on the plan, and get moving.
Let’s not be pleased to announce new tests or new deliveries of equipment. Instead, let’s be displeased until we can announce the plan, set it into motion, and be certain we have enough tests and equipment to meet the need.
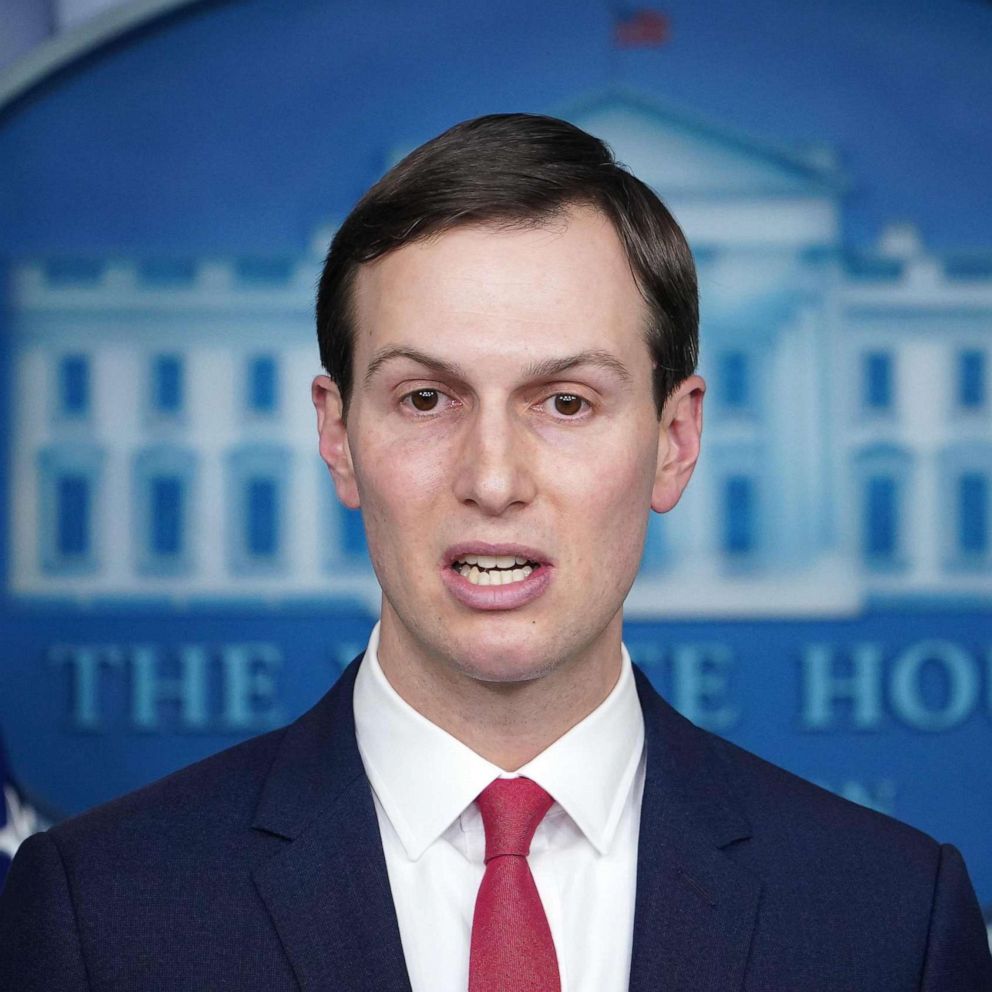
Tom Bossert is a former homeland security adviser to President Donald Trump and an ABC News contributor.