Poverty, pollution and neglect: How the Bronx became a coronavirus 'formula for disaster'
The heavily minority borough has the highest per-case fatality rate in NYC.
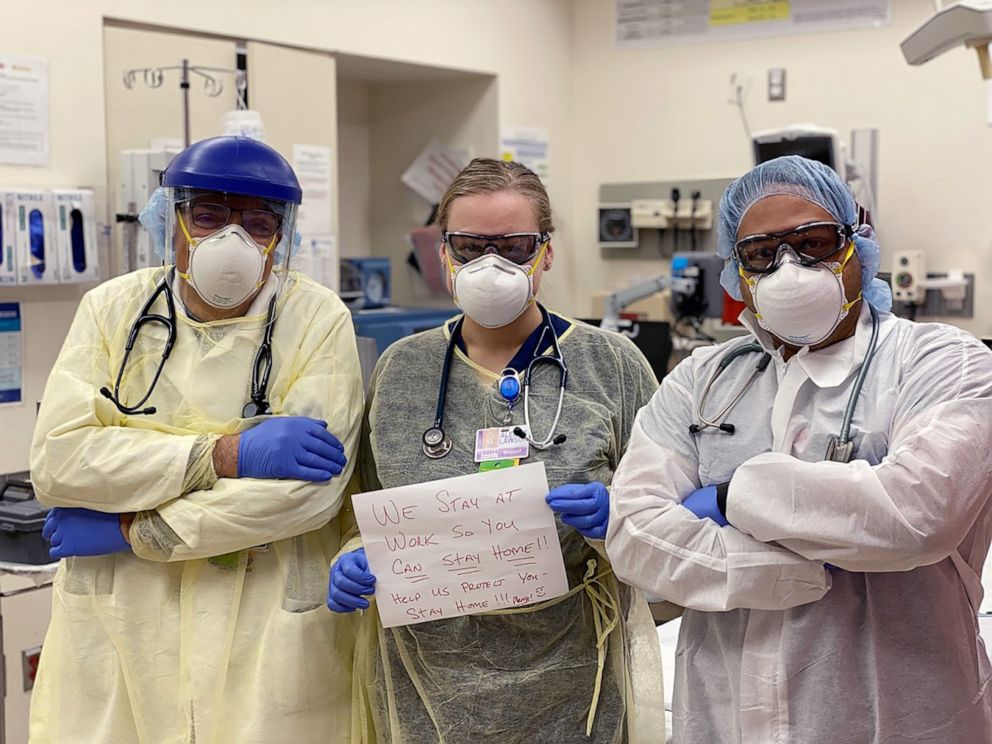
The first thing Dr. Ernest Patti noticed when he stepped into the emergency department at St. Barnabas Hospital in the Bronx for his weekend shift was the sound. An unusually loud cacophony of beepers, alarms and the mechanical gasps of ventilators filled the air.
"The level of noise was unlike anything I've ever heard in the past," the senior attending physician told ABC News. As he began his rounds last weekend, Patti quickly realized it was going to be a ruthless shift. He had begun treating coronavirus patients in mid-March, but now the hospital seemed on the verge of being overrun.
"This truly looked like a war zone. When you went in, the majority of patients [were] in critical condition, lots of people gasping for breath," Patti said.
Over the course of two grueling 12-hour shifts last weekend, Patti says he personally cared for roughly 50 coronavirus patients among the mostly minority and low-income residents the nonprofit hospital serves. He watched four patients succumb to the virus and at one point became seriously concerned the hospital was going to run out ventilators.

The morning before one shift, he recorded a video on his phone where he appears shaken and can be heard saying, "We're gonna have to decide who gets one and who doesn't." The hospital managed to make it through the weekend with enough ventilators and has since been sent more, Patti said. But the ordeal left an indelible mark on him.
"It's really been an unprecedented experience for me and I've been in medicine for 24 years," he said. "You felt helpless."

As the coronavirus crisis unfolds, people across the globe have become familiar with images of an empty Times Square or the Navy hospital ship docked along Manhattan's iconic shoreline. Far less attention, however, has been paid to the Bronx, New York's historically disenfranchised and majority African American and Hispanic outer borough, now suffering under the highest case fatality rate for the coronavirus in the metropolis. Community leaders are calling on the city, state and federal officials to do more to help the besieged and, in their minds, forgotten borough.
Tune into ABC at 1 p.m. ET and ABC News Live at 4 p.m. ET every weekday for special coverage of the novel coronavirus with the full ABC News team, including the latest news, context and analysis.
New York Gov. Andrew Cuomo, New York City Mayor Bill de Blasio and officials from the Federal Emergency Management Agency, all either declined to be interviewed or did not respond to requests for comment for this story.
Representatives from the mayor's office and FEMA, however, disputed that the borough was being ignored in emails sent to ABC News, in part pointing to city-provided food relief and the deployment of National Guard resources across New York City as examples of their efforts.
"We're seeing folks who have struggled before really being hit particularly hard by the coronavirus," de Blasio told reporters on April 8. "Look, that's a blatant inequality and we don't accept it."
"We don't see anyone coming to our rescue"
While the borough of Queens leads the overall death toll in New York City with over 1,600 killed by the virus so far, the Bronx -- which has a smaller population and lower case total -- is seeing dramatically more deaths per case, with 1,185 killed as of April 10, according to New York City Health Department data. The Bronx, home to more than 60% of New York City's very low-income residents, also leads in hospitalizations.
Six percent of Bronx residents who contracted COVID-19 died as of April 7, making them nearly 1 1/2 times more likely to succumb to the virus than the rest of the city, according to public health data analyzed by a Columbia University research lab.
"In terms of the really severe cases, the Bronx is carrying the burden right now," said Micaela Martinez, whose lab at Columbia University's Mailman School of Public Health has been tracking COVID-19's spread across New York City.
Yet, while temporary field hospitals have already opened in Manhattan's Central Park and the Jacob Javits Convention Center, the Bronx's field hospital in Van Cortlandt Park has yet to be completed and isn't expected to be operational for up to three weeks.

"We don't see anyone coming to our rescue or preparing for a potential disaster," said Mychal Johnson, co-founder of the community organization South Bronx Unite. "The community residents here are pretty much living in shock."
The Bronx's plight is just one example of how the virus has disproportionately impacted minority communities around the city and nation. Hispanics accounted for 34% of COVID-19 deaths in New York City though they make up 29% of the population, while African Americans made up 28% of the deaths, but 22% of the population, according to data released by the city. Early data from the Centers for Disease Control and Prevention also shows African Americans are disproportionately shouldering the impacts of the virus nationwide.
New analysis by researchers at New York University's Furman Center, which studies housing, neighborhoods and urban policy, found that the strongest neighborhood factors linked to high COVID-19 rates were having a large share of black and Hispanic residents; having a high proportion of overcrowded apartments and having a large share of residents without college degrees. All three factors are common in the Bronx.
"We need more local options to match the need," Diana Hernandez, a Columbia University public health expert who lives in the Bronx, told ABC News, adding that there's a sense "the [Bronx] population is more invisible and more dispensable, which is to me so unfair."
Hernandez and Martinez are both part of a group of Columbia researchers who, along with South Bronx Unite, have called upon city, state and federal officials to commit more resources to the Bronx. Among their recommendations are increased testing, more portable hospitals and direct food relief for public housing facilities across the besieged borough.
On Wednesday, de Blasio was heckled by Bronx residents demanding more testing as he visited Lincoln Hospital, one of the hardest-hit medical facilities in the city. A spokesperson for the mayor wrote in an email that the mayor had spoken to the individuals afterward and thanked them, telling them their input would "help us to deepen our strategies."
When asked about field hospitals and food relief in the Bronx, the spokesman wrote that the field hospitals were entirely run by the state and federal authorities.
"We had no role to play in selecting locations," the spokesperson wrote in an email to ABC News.
Another spokesperson from the mayor's office highlighted the city's work to feed the needy amid the crisis, saying the city had delivered "over a half a million meals over the last few weeks, with particular strong usage in the Bronx."

Even before COVID-19 struck, nutritious food was hard to find and expensive in many so-called "fresh food deserts" found throughout the low-income borough. The Bronx is New York City's hungriest borough, with 1 in 4 residents experiencing food insecurity in 2018, according to federal data analyzed by Hunger Free America.
The spokesperson said that all residents can look for food relief sites on NYC.gov/GetFood.
A FEMA spokesperson declined to address the issues facing the Bronx or comment on when the Van Cortlandt Park field hospital would be operational, deferring an ABC News interview request to city and state officials, who the spokesperson said are responsible for identifying and approving federal field hospital sites.
State officials should coordinate with FEMA "to register their needs once their capability is exceeded," the spokesperson wrote to ABC News. The spokesperson pointed to the federal government's approval of a major disaster declaration in New York and deployment of National Guard resources as evidence of FEMA's commitment to the state overall.
On Thursday, Cuomo announced the state would open new a walk-in testing facility at health care centers in the South Bronx as part of five new facilities planned in downstate minority communities.
"We are going to increase testing and open new testing sites to collect more data in African American and Latino communities so we can better understand why this virus kills and has higher fatality rates in certain communities, and what we can do to address it," Cuomo said.
The next day the governor addressed the racial disparity of the virus's impact in an interview with co-anchor Michael Strahan on "Good Morning America."
What to know about coronavirus:
- How it started and how to protect yourself: Coronavirus explained
- What to do if you have symptoms: Coronavirus symptoms
- Tracking the spread in the U.S. and worldwide: Coronavirus map
"Are we shocked that the rates are higher in the African American [and] Latino community? We shouldn't be, Michael, if we're being honest," Cuomo said. "We know that there's inequality in the health care system. We know that the poorer communities often pay the highest price for these types of emergency situations because they're really just bringing to light that systemic racism and discrimination in the system."
"Let's learn from this moment," Cuomo continued. "It's testing and understanding why the minority community has a higher rate. Is it because they work in public sector jobs and they were essential workers and they didn't have the luxury, Michael, of staying home? And they didn't have the luxury of going to stay at their second house? Or staying with a relative in their home in the suburbs?"
"There has to be some lesson that we take from this," he said.
Dr. Mary T. Bassett, director of the FXB Center for Health and Human Rights at Harvard University and former commissioner of the New York City Department of Health, told ABC News that while studying the issue was important, "it's really important I think first of all not to act quizzically in this; I'd really like to know who is surprised."
"Secondly, there's no reason to assume this can't be changed," she said. "I don't think you need to study things to see that more resources must go there."
"We don't have time for another study of race and disparity in the South Bronx," Johnson, of South Bronx Unite, wrote to ABC News in response to the state and city actions taken so far to address his community.
"We need immediate, concrete, lifesaving measures to mitigate the documented threat right now," he wrote.

'It's just a formula for disaster'
Deciphering further exactly why the Bronx is suffering so disproportionately will take time, but decades of environmental health concerns and structural neglect have left Bronx residents especially vulnerable to COVID-19, community leaders and health experts told ABC News.
"The situation in the Bronx with respect to COVID is really about the reality before COVID," Hernandez said. She noted her neighborhood's long-standing high poverty rates, poor health care access, systemic environmental degradation and dense public housing as just some of the key factors allowing the virus to wreak havoc across the borough.
"It's just a formula for disaster," Hernandez said.
Home to the poorest congressional district in the country and what researchers say is the unhealthiest county in the state of New York, the Bronx has long been plagued by underlying illnesses now associated with an increased vulnerability to COVID-19, such as respiratory problems, diabetes and heart disease. More than 91% of Bronx residents who died from COVID-19 had underlying conditions as of April 10, according to New York City Health Department data.
For decades, the borough suffered under some of the worst air pollution in New York City. The Bronx contains seven of the city's top-10 neighborhoods for asthma rates, according to an analysis by housing-data website Localize.city. The Morrissiana/Highbridge neighborhood, home to the city's second-highest asthma rate, is now among the city zip codes worst hit by the coronavirus, according to health department data.
As COVID-19 deaths continue to rise in the Bronx, Johnson said many residents feared their historically polluted air had left them particularly vulnerable to the virus.
New research released by Harvard this week appeared to put hard data to that fear and illustrated a link between chronic air pollution and American coronavirus deaths. The research showed that nationwide, counties with higher levels of chronic air pollution were experiencing a substantially larger number of COVID-19 deaths. An increase in just one unit of particulate matter air pollution was associated with a 15% increase in the COVID-19 death rate, the research found.
"It's becoming more and more clear that the virus is really attacking your lung function," Francesca Dominici, senior author for the Harvard research, told ABC News. "And if the respiratory system is already inflamed because of pollution it's like you're putting gasoline on the fire."
The South Bronx, often described as "Asthma Alley," is surrounded by four highways, several waste facilities and a steady stream of heavy truck traffic servicing a nearby Fresh Direct warehouse, the printing press of The Wall Street Journal and other diesel-intensive industries that fill the streets with emissions.

"You couldn't find a location that's more designed for mortalities than the community we live in," Johnson said.
The area's pollution woes stretch back to the era of Robert Moses, the powerful city planner who presided over New York for 44 years stretching back to the 1920s, often running expressways straight through low income and minority neighborhoods. Moses and subsequent other city planners ultimately surrounded the Bronx with a constant stream of auto-emissions that would persist decades. The expressways were then followed by other industries considered too undesirable for Manhattan.
"For decades we've been the dumping location for fossil fuel power plants, waste transfer stations, heavy diesel truck intensive business and highways that serve other neighborhoods," Johnson said. "We were forced to shoulder the burden of these businesses for supposed economic development, but we never saw it trickle down, we only saw the health effects."
"We know air pollution exacerbates asthma," Markus Hilpert, an associate professor at Columbia University who has been studying the health impacts of air pollution in the South Bronx for years, told ABC News. "The chances of getting severely sick from the [COVID-19] virus or even dying depend very much on preexisting conditions, such as respiratory disease. ... We have a very high prevalence of asthma in the South Bronx, and because of that I'm very concerned about residents living in this area."
Patti, the doctor at St. Barnabas Hospital in the Bronx, saw the effects firsthand.
"We were seeing folks who'd come in with asthma or emphysema, those folks were definitely coming in [with] a high proportion of respiratory stress," he said. "When you already have a damaged set of lungs and you come into a hospital with a virus that is primarily affecting your respiratory tract, your lungs, you [have] a higher risk of going into respiratory failure."

New York City Council Member Rafael Salamanca Jr. said asthma was a "huge issue" in the South Bronx, which he represents. It's also an issue close to him, as both he and his 5-year-old son are asthmatic. Then, just last week, his father, a long-time Bronx resident, passed away from the coronavirus.
"It hit directly home," Salamanca said. "My community is really the most at risk in this epidemic and to be honest it's scary, it's really scary."
Salamanca was among the 10 South Bronx elected officials who sent a letter to state Cuomo's office earlier this week, asking for the state to immediately expand "testing and hospital services" in the South Bronx. The officials asked that a field hospital be established in the Harlem River Yards, a state-owned, 8-acre waterfront site.
"If New York State cannot accommodate this request, we ask that you convey the rationale as to why and that you request assistance from the federal government to activate this proposal," the officials wrote. The officials said they have yet to receive an answer as of this report. A FEMA spokesperson declined to comment on whether the agency was aware of the request.
Clean air under threat nationally
As researchers continue to probe links between air pollution and coronavirus deaths, many have expressed alarm at the Trump administration's decision to relax Environmental Protection Agency monitoring and not impose pollution fines during the crisis. Just last week, the administration also weakened Obama-era rules to compel auto companies to produce more fuel-efficient vehicles.
Heather McTeer Toney, a former EPA regional administrator and national field director for anti-pollution group Mom's Clean Air Force, told ABC News such decisions were "inhibit[ing] the wellness of the American public."
"Creating worsening air pollution is something that we just can't deal with right now," she added.
An EPA spokesperson told ABC News by email that the changes were "not a blanket waiver of enforcement" and that the agency "does not expect any increase" in air pollution levels as a result. As of this report, the agency has not indicated when it plans to end the relaxation period.
Nearly 141.1 million people in the U.S. are already exposed to unhealthy air, with more than 4 in 10 people living in counties with unhealthy ozone or particle pollution, according to the American Lung Association's 2019 State of the Air report.
Mustafa Santiago Ali, a former EPA official who helped create the agency's environmental justice office, said it's often struggling communities that feel the brunt. He said that often talks about "sacrifice zones" around the country where communities of color, low wealth and indigenous peoples are exposed to higher levels of pollution that contribute to chronic health problems that make people more susceptible to COVID-19.
"We call them sacrifice zones because they're the areas that you know there's been disinvestments, they're in the areas that there's been lack of enforcement," he told ABC News. "And truly, one of the main factors on the underneath of it unfortunately is systemic racism and discrimination."
As the coronavirus exposes the potentially deadly divides in American cities, Hernandez, of Columbia University, said the issue extends beyond the South Bronx.
"This is about front line communities in all states," Hernandez said.



