It takes a community to help overcome vaccine hesitancy: OPINION
Community health centers care for approximately 30 million Americans.
President Biden's five-point plan to speed up vaccine distribution to hundreds of millions of Americans this year, may help close the chapter on a dark period in the U.S.
One area of emphasis in Biden's plan is related to community health centers.
Right now, limited supply is the major roadblock to mass vaccinations - with pent-up demand immediately zapping limited supply. Furthermore, even if enough supply existed, community health center staff and patients find it difficult to access as the supply has been typically sent to hospitals and other distribution points. But once the supply problem eases, the Biden administration will face another major hurdle: vaccine hesitancy, particularly in underserved communities where distrust, fear of illness and lack of literacy are strong barriers.
The Trump administration also had a plan to address the problem of vaccine hesitancy. But the Biden administration now has the opportunity to tackle one of America's greatest challenges head-on and community health centers will be a key partner in that effort.
Vaccinations move at the speed of trust, empathy and inclusion. A key aspect of Biden's plan involves a clear communication strategy to overcome vaccine hesitancy and misinformation as well as tapping into the nation’s networks of community health centers which care for approximately 30 million Americans in rural and urban communities across the country, according to a report from the National Association of Community Health Centers.
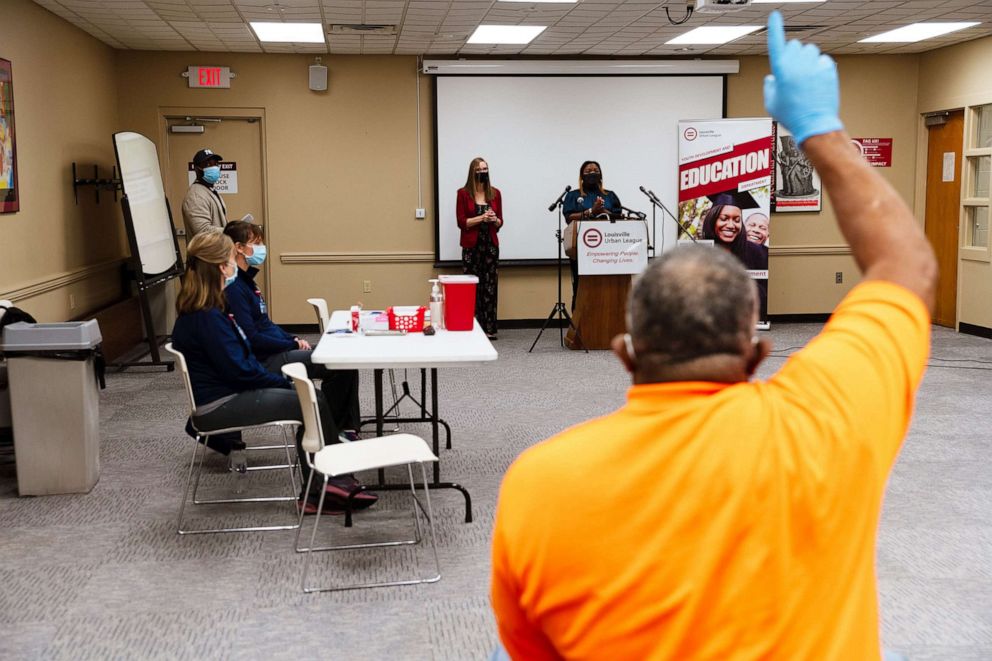
Both objectives can and should be met by activating primary care clinicians and their teams in community health centers around the country to combat the virus. There is a need to accelerate vaccinations and battle misinformation at the point of care in communities with trusted and credible messengers.
Only 40% of older Black adults and 51% of older Hispanics said they are somewhat or very likely to get the COVID-19 vaccination -- compared with 63% of older white people, a University of Michigan poll shows. They are concerned about efficacy and safety.
Studies have illustrated that changing behavior especially around health care decision-making is often best done at key inflection points, for example, patients are more likely to quit smoking when counseled upon discharge from the hospital or change their diet after a hospitalization for diabetes or a heart attack.
The same can be said about trying to help high-risk communities consider vaccination against COVID-19. Community health centers serving those disproportionately impacted by the pandemic are often staffed by clinicians who are members of the community as well. Given the incredible concerns around the pace of vaccination and a looming threat of a more transmissible virus becoming dominant in the coming months, any and all innovative efforts should be explored, a sentiment echoed by the incoming Biden leadership.
Here are five ways to overcome hesitancy through community health centers:
1. Enhance flexibility in fighting misinformation.
Encourage state and local authorities to allow for flexibility in developing information regarding common facts and myths around the vaccine in conjunction with vaccine distribution consistent with science and Centers for Disease Control and Prevention guidance. Community health centers can offer information during the course of important primary care visits even if the patient or family member is not currently eligible for the vaccine. The conversation started there can be continued via text messaging similar to national efforts such as text4baby.
2. Take a data-driven approach.
Distribute doses to community health centers in proportion to the populations they serve and how they have been impacted to date consistent with risk. Many health centers have experienced incredibly high positivity rates while serving as primary testing centers, offering an incredible access point as facilitators and trusted partners for mass vaccination clinics.

3. Eliminate barriers to access.
Very often, issues such as transportation, hours of operation, etcetera, are often barriers to health care access. By building on the information that most community health centers already know, barriers can be eliminated proactively. Mobile vans and clinics in high-risk communities can help in vaccination efforts within those communities. Church parking lots could be another familiar place for sharing information, building trust and delivering the vaccine. Health centers have partners such as churches, community stakeholders, barbers and hair stylists, and revered teachers. All can be important agents for change.
4. Engage nontraditional partners of community health centers.
Many CHCs have an incredible relationship with area food banks, schools and local businesses, these are all important distribution channels for information as well as a mechanism to engage communities on their terms and in their context.

5. Create a patient ambassador corps for the community.
Health centers can identify, train and support patients who have taken to plan to take the vaccine as effective messengers. By using their influence, stories and trust they can motivate others in the community who may be skeptical about the vaccine. Their stories could be shared online, via a digital community portal for example, to help allay fears of vaccinations. These stories can also be used by health care workers in community health centers to motivate their colleagues and patients to get vaccinated.
Overcoming vaccine hesitancy requires time, commitment and meeting communities where they are at. We are at a critical moment and delivering on vaccinations in communities disproportionately affected will go a long way in beating COVID-19.
Jay Bhatt is an internal medicine physician, an instructor at the University of Illinois School of Public Health and an ABC News contributor. Kavita Patel is an internal medicine physician and senior fellow at the Brookings Institution.



