How Wyoming became the most vaccine-hesitant state
The percentage of reluctant residents in Wyoming is double the national average.
With more than half of U.S. adults now having received at least one dose of COVID-19 vaccine, the country is on the precipice of a new vaccination challenge: hesitancy.
According to new estimates from a U.S. Census Bureau survey conducted from October to March, we know more about which Americans are most likely to say they're "definitely not" or "probably not" going to get a vaccine once it's available to them.
Wyoming has emerged as the most vaccine-hesitant state in the country -- an estimated 33% of adults said they were are reluctant to get a COVID-19 vaccine, compared with an estimated 16% of nationwide.
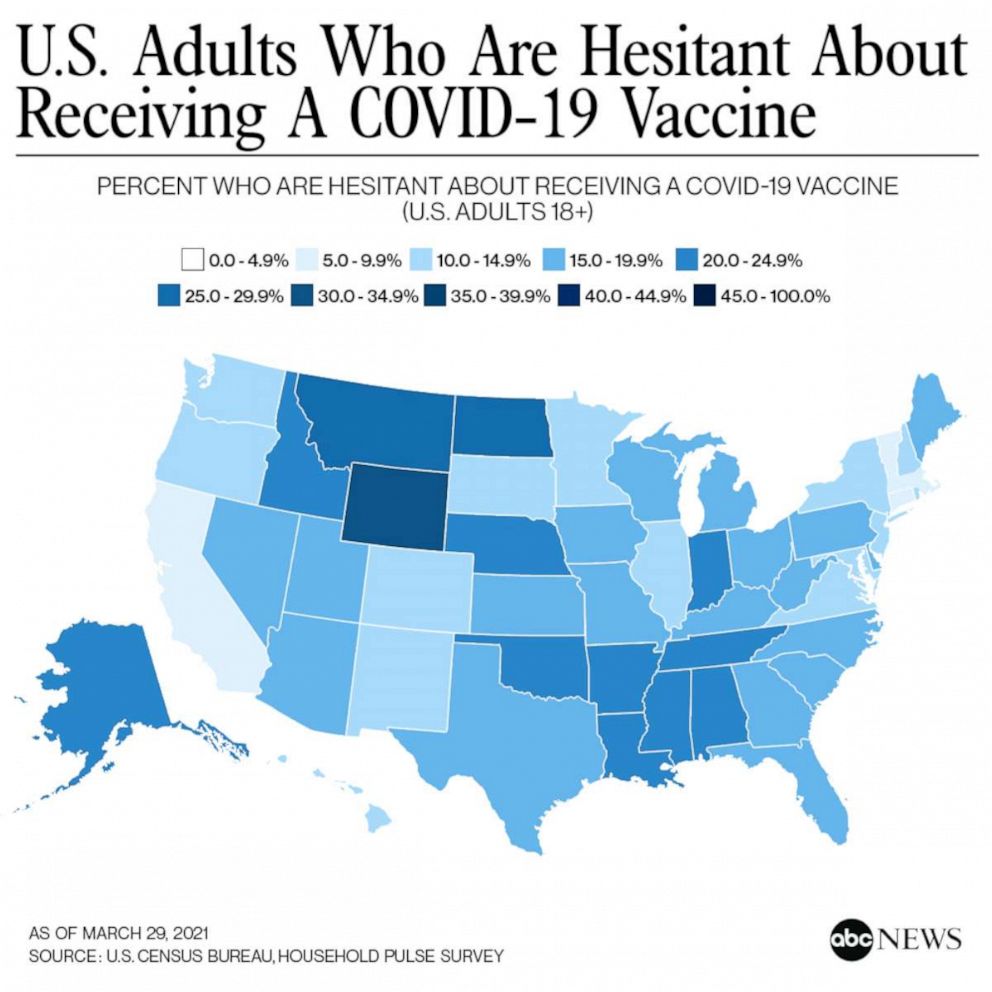
According to an ABC News analysis of county-level data, vaccine hesitancy is estimated to be higher in rural areas, particularly in the West and South. Counties with high estimated hesitancy also tend to be younger, poorer and more likely to have been won by former President Donald Trump during the 2020 presidential election.
Vaccine hesitancy estimates in Wyoming's neighboring states outpaced most other areas of the country. In Montana, North Dakota and Idaho, roughly a quarter of residents were reluctant to get vaccinated, compared with 8% of residents in Connecticut.
The top three reasons cited for vaccine hesitancy in Wyoming were "Concerned about side effects," "I don't believe I need it" and "Don't trust COVID-19 vaccines," according to the survey data.
Linda Thunstrom, an associate professor of economics at the University of Wyoming, said the Census Bureau survey tracked with research she's conducted with the help of Madison Ashworth, a Ph.D. student, and others on her team. Those findings aren't yet published, but preliminary indications are that vaccine hesitancy in Wyoming might be more persistent than it is nationally. Still, she added, the main drivers of vaccine hesitancy tend to be similar across the U.S. -- people are worried about side effects and about the vaccine being so new.
A third important factor appears to be "low trust in government agencies and also in the companies that develop the vaccines," she said.
What's happening in Wyoming?
In Wyoming, where 42% of adults have received at least one dose of a vaccine compared with 51% of adults nationally, according to the Centers for Disease Control and Prevention, state-based health experts offered a variety of theories for why some patients may eschew a vaccine, ranging from mixed public health messaging to concerns about safety to a belief that the worst of the pandemic has passed.
"Wyoming has had low levels of COVID-19 illnesses and hospitalizations for a while now, which affects threat perception," said Kim Deti, a spokesperson for the Wyoming health department. The state saw its biggest spike in COVID-19 cases in November and December, according to state health department data, and is now reporting fewer than 50 new cases each day.
"I think part of the issue goes way back to when the pandemic started," said Dr. Jeffrey Chapman, chief medical officer at Cheyenne Regional Medical Center, adding that the messaging over mask wearing was well-intentioned but inconsistent. "People just don't know what to believe anymore."
Linda Van Dorn, who directs Cheyenne Regional's COVID vaccine clinic, said some patients who come in for vaccines ask, "How safe is it really? How effective is this?"
Others have asked whether the vaccine contained a live virus. (It does not.) And despite an Axios/Ipsos poll this month, which found the Johnson & Johnson vaccine pause had not affected Americans' likelihood to get vaccinated, Van Dorn said patients have asked about the pause.
"The shot that you are giving me today is OK, right?" she recalled patients asking.
The Johnson & Johnson pause, Chapman said, is similar to the messaging over masks: "Things just change all the time, which just creates angst."
Still, Van Dorn emphasized that Cheyenne, the state's capital and home to about 65,000 people, was doing much better on vaccinations than surrounding areas.
"The people that are coming in, they don't have that same sense of hesitancy that we're hearing about from our rural counties," Van Dorn added.

For Wyomingites on the fence about getting vaccinated, Chapman said a primary concern was long-term safety of a new vaccine. In younger populations, lower personal risk of severe COVID-19 complications was a factor, with some people, according to Chapman, saying things like, "I'm 20-some years old. All my friends have gotten COVID and it was just a cold. Why should I take any risk at all?"
Faced with those concerns, Chapman emphasized the importance of vaccination for the community at large.
"This isn't just about the individual getting the vaccine," he said. "This is about a community effort to try and eliminate the virus so we can get back to normal."
Rugged individualism meets limited health care access
The individualism that Chapman described can cut two ways, according to Noel Brewer, a professor of health behavior at UNC Gillings School of Global Public Health.
"People who live in rural areas are used to being self-sufficient," Brewer said. "In places where physicians and other health care resources have been scarce, it's common to be a bit entrepreneurial about your own health. You see that in rural areas all across the country."
On the other hand, people who live in areas where health care is limited or hard to access may be more inclined to see vaccines as a valuable tool. "The idea of having a prophylactic against future harm that allows you to not have to go to the doctor can be extremely appealing," Brewer said.

When it comes to increasing vaccination rates among the hesitant, Brewer said there are additional factors to consider beyond how people feel about vaccination. He pointed to the Increasing Vaccination Model, adapted by a World Health Organization working group based in part on Brewer's research, which is meant to identify behavioral and social drivers of vaccination.
Three factors play into whether people get vaccinated, according to the model: what people think and feel; social experiences and norms; and practical issues, like their ability to schedule an appointment or pay for it.
"It's very common for people's intuition and for studies like this to reflect what people think and feel," Brewer said. "The reality is that the most influential factors are often the practical factors."
In the case of the COVID-19 vaccine, "The main barrier right now that people face is the fact that vaccination appointments are hard to sort out," he said, adding that complex online appointment systems represent are a barrier to vaccination.
In Albany County, Wyoming, Christine McKibbin, director of the Wyoming Center on Aging, is trying to address that barrier head-on. McKibbin and her team helped staff a COVID-19 call-in center for the first eight weeks of its existence, so that people without access to the internet, or who weren't tech-savvy, still could make vaccine appointments.
People who contacted the call center were eager to get vaccinated, she said. "The vaccine is seen as a pathway for them to be able to see family again or gather in small groups together, potentially to travel again."
Olivia Davies, a fourth-year student at the Medical College of Wisconsin and who will be starting her residency at Massachusetts General Hospital this summer, is a contributor to the ABC News Medical Unit. ABC News' Mark Nichols, John Kelly, Cindy Galli and Brian Hartman contributed to this report.







