Artificial 'biobag' womb for extremely premature newborns in testing
Researchers at Children's Hospital of Pennsylvania revealed the new device.
— -- Infants born extremely prematurely face a host of health issues from underdeveloped lungs that can cause chronic lung damage to fragile blood vessels that can cause bleeding in the brain.
For decades, doctors in the neonatal intensive care unit have done their best to mimic the complex environment of the womb as they work to keep these tiny infants alive.
This week, researchers at the Children's Hospital of Philadelphia revealed a new device that could help save the lives of the smallest patients, in a study published in Nature Communications. The device acts as an artificial womb using a "biobag" to mimic the natural uterus that allows a fetus to develop.
"These infants have an urgent need for a bridge between the mother’s womb and the outside world," Dr. Alan W. Flake,a fetal surgeon and director of the Center for Fetal Research at Children’s Hospital of Philadelphia (CHOP) said in a statement released yesterday.
"If we can develop an extra-uterine system to support growth and organ maturation for only a few weeks," he added, "we can dramatically improve outcomes for extremely premature babies."
Currently, the device is in the animal testing phase of development and more work will need to be done before it can be approved for testing on human infants.
When infants are born severely prematurely -- between 23 and 25 weeks -- their chances of survival, without ongoing complications including lung or brain problems, is low. That's due, in part, to their underdeveloped lungs, liver, kidney and brain that are forced to start working months earlier than normal.
"Everything is formed at that stage but is very, very immature," Dr. Jonathan Fanaroff, from the NICU at University Hospitals Rainbow Babies & Children's Hospital, who was not involved in the study, told ABC News. "Our job in the NICU is to support growth and minimize harm."
In hopes of building a better incubator, the team at CHOP created multiple prototype devices, eventually creating a device that features a biobag filled with amniotic fluid and a machine to oxygenate the blood via the umbilical cord.
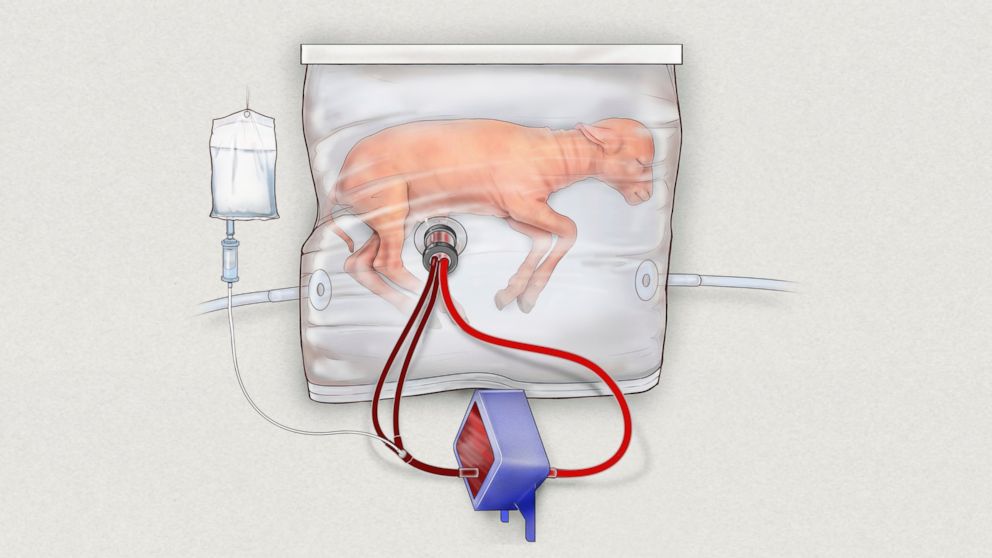
An important part of this incubator, or extra-uterine support device, is the ability to sustain infants without using a ventilator, which can strain their underdeveloped lungs or cause scarring that leads to chronic lung disease.
By connecting the umbilical cord to a gas exchange that oxygenates the blood, the device function is similar to how a fetus "breathes" in the womb via the umbilical cord. The biobag is kept in a temperature controlled, near-sterile environment with the infant submerged in amniotic fluid. The device also allows researchers to monitor key vital signs and blood flow, so that doctors can respond quickly if the patient starts to deteriorate.

To see if the device might work on humans, researchers used lambs born at a gestation between 105 to 120 days, which is somewhat equivalent to a human infant born between 22 to 25 weeks. Using the most current device they developed, researchers measured how long eight prematurely born lambs survived in the device and grew. The animals were also tested to see if they were developing normally.
Five of the eight animals born between 105 to 108 days gestation lived between 25 and 28 days and three animals born at 115 to 120 days lived between 20 and 28 days in the device. The longest an animal was in the device was 28 days and the researchers stopped the experiment at that point, due to animal testing protocols, rather than a poor health outcome.
While the study is small and the findings preliminary, the researchers are hopeful that this device could be the future of caring for preterm infants that would be less taxing than current methods.
"This system is potentially far superior to what hospitals can currently do for a 23-week-old baby born at the cusp of viability," Flake said. "This could establish a new standard of care for this subset of extremely premature infants."
Dr. Jonathan Fanaroff from the NICU at University Hospitals Rainbow Babies & Children's Hospital, said should the device prove to be effective in humans as well as animal testing it could be a "major advance."
"I think it's very exciting. You know, in a lot of ways this is what we're trying to do in the NICU today, we're trying to do our best to mimic the environment they have in the womb," Fanaroff said. "This looks like the next step."




