COVID-19 pandemic vs. endemic: What's the difference, and why it matters
Experts say they’re not ready to call the coronavirus endemic just yet.
The United States marked a new stage in the government's response to the COVID-19 pandemic when President Joe Biden announced in his State of the Union address Tuesday that "COVID-19 no longer need control our lives."
The World Health Organization declared a global pandemic in March 2020 due to rapid spread of COVID-19 all across the globe.
However, as many experts believe the virus that causes COVID-19 will never be eradicated, the world must at some point transition away from “pandemic” and toward an “endemic” phase.
Pandemics are a widespread, rapid spread of disease, with exponentially rising cases over a large area. Endemic viruses, meanwhile, are constantly present and have a fairly predictable spread. That predictability allows health care systems and doctors to prepare and adapt, reducing loss of life.
For a pandemic to reach an endemic phase, it would need to be "a situation where you have a background level” of disease, said Dr. Daniel McQuillen, president of the Infectious Diseases Society of America and a senior physician in the division of infectious diseases at Beth Israel Lahey Health in Massachusetts.
This means that, while some people would still get infected, it wouldn't be an unbearable number with devastating consequences that overwhelms the public, hospital systems and providers.
The seasonal flu, or influenza, is an example of an endemic virus. H1N1 influenza has had pandemic spread of variants in the past, such as the Spanish flu in 1918 and swine flu in 2009. Variants of these are now part of respiratory viruses that we encounter regularly.
“There’s not a hard and fast rule for when a pandemic becomes an endemic,” said Dr. Paul Goepfert, a professor of medicine in the University of Alabama at Birmingham's division of infectious diseases.
Without knowing if there may be another variant on the horizon and without a predictable pattern of disease, it’s still too soon to tell if the nation has reached an endemic phase.

That's why many Americans are concerned it’s too soon to lift mask mandates. There is still a lot of transmission, and young children and immunocompromised people are still vulnerable.
However, McQuillen said the new CDC guidelines are a reasonable shift, as they focus on local transmission and capacity.
“We’re going from trying to prevent disease completely to going more to how do we deal with preventing severe illness and hospitalizations and how do we prevent our health care system from getting so swamped that we can’t take care of even normal problems,” he said.
This must be determined at a local level.
“I think [the new CDC guidance] reflects this need to be flexible in how to respond to the pandemic,” said Dr. Natasha Chida, assistant professor in the division of infectious diseases at Johns Hopkins University.
Pandemics are “not a static experience,” she said. Some places in the country still have very low hospital capacity, so they would struggle to handle additional cases and thus would benefit from masking. But when numbers are low, we should “be able to have a normal type of experience,” she said.
Despite the new guidelines, many experts are hesitant to say the nation has entered an endemic phase just yet, as only time will tell if a new variant will arise and cause similar upheaval.
“Endemic is where you are seeing consistently low numbers, the health care system is able to manage it [and] people are able to get the care they need,” Chida said.
While the U.S. is getting close, numbers have dropped before and then new variants emerged, so it’s “too soon to say” if we are in this phase yet, she said.

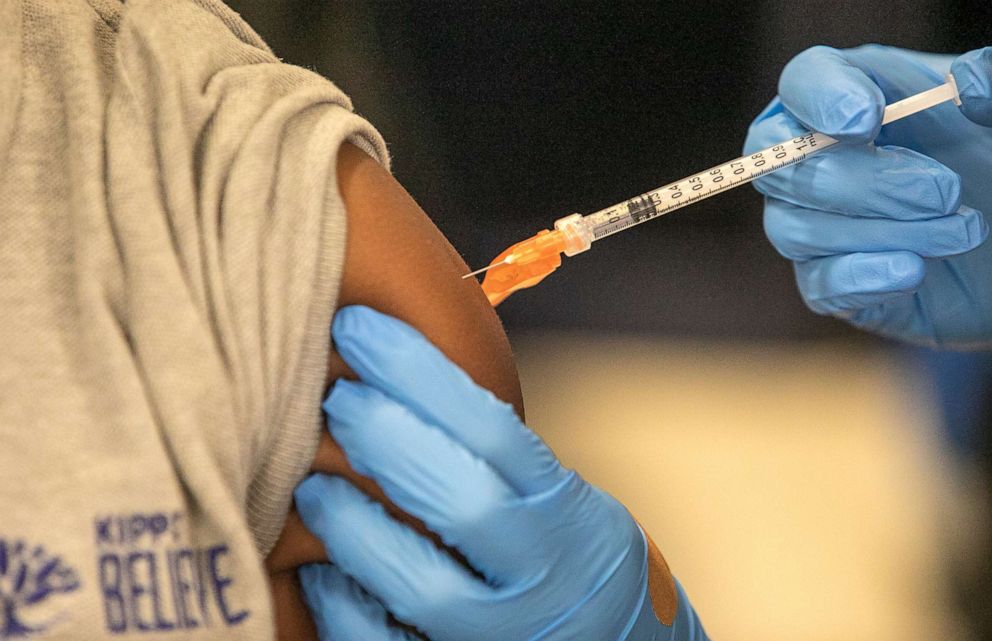
To prepare for and prevent another wave, McQuillen, Goepfert and Chida each emphasized the importance of building better infrastructure for public health initiatives. This includes equitable vaccine distribution across the globe and increasing supply of treatments and testing -- items currently outlined in the White House’s new pandemic policy agenda.
Goepfert also noted the importance of supporting primary care providers, both in allowing them to administer vaccines in their clinics and ease of access to treatment.
“What the pandemic laid bare was that public health has been massively under-resourced for decades, and people suffered because of that,” Chida said.
Now, with more than 75% of Americans vaccinated, experts are hopeful that the country can move toward better control of the disease and toward a new endemic phase -- where we can control the disease, and it doesn’t control us.
Emily Molina, MD, an internal medicine resident physician at the Johns Hopkins Hospital, is a contributor to the ABC News Medical Unit.




