Feds unveil plan to 'reduce suffering' for nursing home residents and staff amid COVID-19 pandemic
Some advocates say report does little to set higher standards for nursing homes.
An independent commission set up by the Trump administration has unveiled a host of recommendations it says could help nursing homes "reduce the suffering and to save the lives of residents and staff" as they continue to wage a deadly battle against the coronavirus, though some critics say the commission didn't go far enough to help America's most vulnerable because it does not address enforcement of federal quality of care standards.
In April, as the coronavirus pandemic swept through nursing homes across the country, Seema Verma, head of the Centers for Medicare & Medicaid Services, announced the commission would be tasked with enhancing strategies for infection control and prevention and strengthen protocols to identify COVID-19 in facilities and mitigate its spread. The commission was made up of 25 appointed members, including infectious disease experts, directors and administrators of nursing homes, academics, state authorities, clinicians and a nursing home resident.
In its final report released on Wednesday, six months later, the independent task force laid out 27 recommendations with an emphasis on a national testing strategy, providing facilities with at least three months’ worth of personal protective equipment and continuing to ensure proper units are available for infected or possibly infected residents.
The 186-page report also calls for better communication among residents, staff and families, increased registered nurse and infection preventionist presence in facilities, more professional development opportunities for certified nursing assistants and a stronger long-term care infrastructure.

“The Commission urges CMS, as the lead federal agency with nursing home quality and safety oversight, to lead, to advocate, and to ensure accountability for nursing homes and their residents and staff in the national pandemic response,” the commission wrote.
While the report does not explain how the recommendations will be funded, the commission noted that some members voiced strongly that CMS should make no unfunded mandates. "If CMS implements the recommendations and actions steps in this report, it must do so in a way that ensures funding mechanisms are in place to support them," the commission wrote.
Nursing homes have been especially devastated by the coronavirus pandemic. Almost 12,000 facilities nationwide have reported COVID-19 among their residents and staff, which has led to more than 50,000 deaths among residents in long-term care facilities, according to CMS.
In the report, the commission noted that the recommendations will likely be inadequate to enable nursing homes to prevent the next crisis unless accompanied by a more general “sustainable, systems-level change." The commission wrote that nursing homes need to be “reimagined to ensure they can protect the safety and foster the well-being of some of the most vulnerable members of our population.”
“The time has come for a turning point in nursing home care. The Commission envisions a person-centered, resilient system of care that is better for the next generation — one that more deeply values and respects older adults and people with disabilities as vital to the fabric of American society,” the commission wrote.
Although, the recommendations made to CMS are not legally binding, Jeannee Parker Martin, the President and CEO of the elder advocacy group LeadingAge California and one of the commission's members, said that CMS will decide which of the recommendations are most critical to undertake immediately.
In a press release, CMS said the commission’s findings align with the actions the Trump administration and CMS have taken to contain the spread of the virus and to “safeguard nursing home residents from the ongoing threat of the COVID-19 pandemic.”
“The Trump Administration’s effort to protect the uniquely vulnerable residents of nursing homes from COVID-19 is nothing short of unprecedented,” said CMS Administrator Seema Verma. “In tasking a contractor to convene this independent Commission comprised of a broad range of experts and stakeholders, President Trump sought to refine our approach still further as we continue to battle the virus in the months to come. Its findings represent both an invaluable action plan for the future and a resounding vindication of our overall approach to date.”
But some nursing home advocates say the report does little to set higher standards for nursing homes.
Eric Carlson, directing attorney at Justice in Agin and one of the Commission’s members, did not endorse the report, saying it failed to address enforcement of federal quality of care standards.
“With limited exceptions, these recommendations and action steps do not address accountability of nursing homes and their operators,” said Carlson in a statement. “The result is an imbalanced report that gives a misleading impression of CMS’s role. “
Michael Brevda, an attorney at the Boca Raton-based Senior Justice Law Firm echoed those sentiments.
“The Commission’s Final Report misses an opportunity to create and enforce real nursing home quality standards,” Brevda told ABC News. “ Administrative fines for adverse incidents like bedsores, medication mistakes and fall injuries would greatly deter bad nursing home care.The woefully unregulated nursing home industry we’ve lived with for decades has been plagued with bad actors and poor resident care.”
“We can change this through legal accountability,” Brevda continued. “Sadly, the Commission's Final Report misses the mark.”
For Toby Edelman, a senior policy attorney for the Center for Medicare Advocacy, a nonprofit that provides legal assistance for the elderly, the report is “far too easy” on both nursing facilities and the federal government.
“The report essentially treats nursing facilities as having no responsibility for the tens of thousands of resident and staff deaths,” Edelman told ABC News. “This kid-glove treatment is not justified when research studies document that facilities with better staffing levels have fewer cases and fewer deaths.”
“During the pandemic, the federal government has largely taken a hands-off approach,” Edelman continued. “....it left states and facilities on their own to respond to the crisis – to figure out appropriate practices, to get and require testing of residents and staff, to get and use personal protective equipment.”
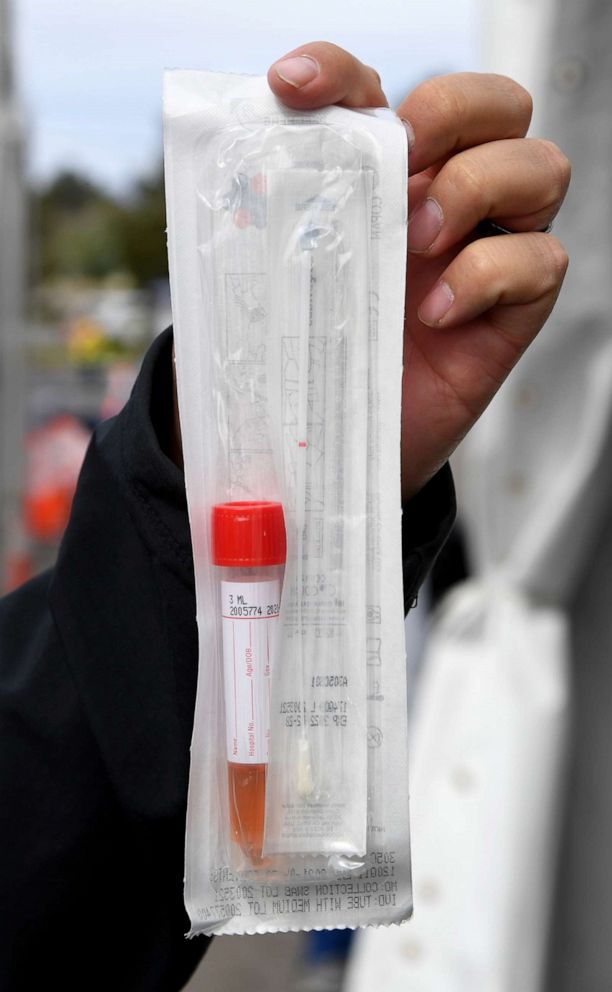
In August, a new mandate by CMS required nursing homes to test all staff and conduct widespread testing among residents. Nursing homes that fail to test residents and staff could face fines under the measure announced by the Trump administration. Federal agencies announced they would provide point-of-care testing kits to 15,000 nursing homes around the country. A spokesperson for CMS told ABC News last week that just over 13,000 machines and nearly 5 million point-of-care tests have been shipped to 13,343 facilities so far.
What to know about coronavirus:
- How it started and how to protect yourself: Coronavirus explained
- What to do if you have symptoms: Coronavirus symptoms
- Tracking the spread in the U.S. and worldwide: Coronavirus map




