COVID-19 testing disparities evident in San Antonio and Dallas areas: ANALYSIS
Communities of color often have longer wait times, understaffed testing centers.
Kenneth Hamilton, 31, had been waiting for four hours in the line to take a COVID-19 test at Houston’s NRG stadium.
Eventually, after spotting several people not wearing masks or social distancing, Hamilton — a small business owner and father of seven — decided that continuing to wait wasn’t worth the risk of being exposed to coronavirus in the line itself. So he left, and looked for other testing options in his neighborhood.
But as a Black resident of Houston’s Third Ward, the line Hamilton left was, at the time, his only nearby option. Three months after he first sought a test, he says there are considerably more testing centers in his neighborhood.
“One of the schools that my kids go to, and one of the schools close by in the neighborhood, and a couple of churches now have them,” he said. “They ramped up, to an extent.”
The Houston urbanized area is just as diverse as many other major Texas metropolitan areas, but the city’s initial plans to spread testing centers out equally across its neighborhoods while still operating at capacity helped to reduce site demand. As a result, the community demands of various neighborhoods were fairly equal. ABC News and FiveThirtyEight’s analysis showed that, on average, predominantly Black Houston neighborhoods faced similar levels of potential need as white neighborhoods. Hispanic neighborhoods had slightly higher potential community need than white neighborhoods, but not by much.
But the disparities are still clearly visible in San Antonio and Dallas areas.
According to a new, extensive review of testing sites by ABC News, FiveThirtyEight and ABC-owned television stations, sites in communities of color in many major cities face higher demand than sites in whiter or wealthier areas in those same cities. The result of this disparity is clear: People of color, especially Blacks and Latinos, are more likely to experience longer wait times and understaffed testing centers.
This nationwide review is one of the first to look at testing site locations coast to coast, in all 50 states plus Washington, D.C., using data provided by the health care navigation company Castlight Health (the same data that Google Maps uses to surface COVID-19 testing sites). An assessment of city and state health department websites also revealed, over and over, fewer testing sites in areas primarily inhabited by racial minorities.
Importantly, our analysis does not factor in the capacity of testing sites -- which can vary from just 50 tests at one site to 2,000 at another, meaning that one site might be equipped to serve a larger number of people than another site. Instead, it looks at the potential demand for each site based on the number of people and sites nearby. The data we used also is less likely to reflect tests done in private physicians’ offices than federally-funded community sites, local government-run mobile pop-up sites, urgent care clinics and hospitals. The analysis also doesn’t take into account other factors that could determine testing accessibility, such as staffing and wait times, as well as other restrictions on testing like appointment or insurance requirements.
San Antonio
In the San Antonio urbanized area, testing sites in poorer, majority-Black and majority-Hispanic neighborhoods in the south, east and west are estimated to have to serve far more people than sites in more affluent, whiter neighborhoods in the north, resulting in a disparity in potential community need.
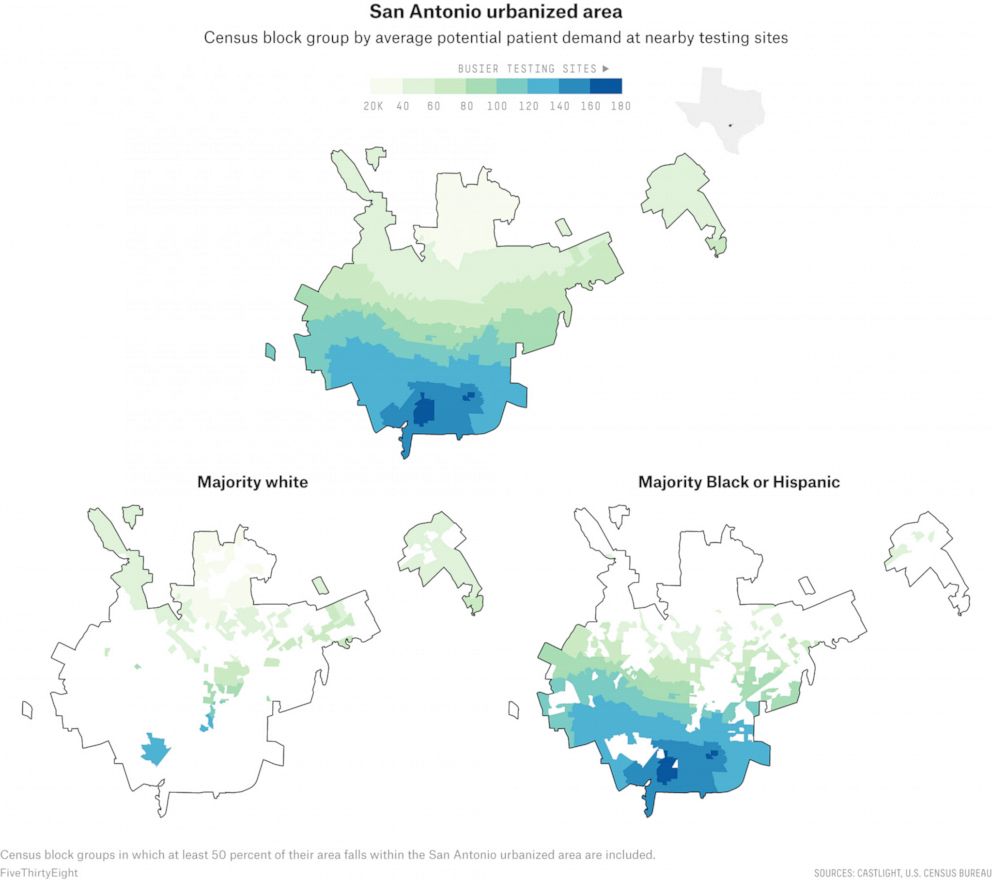
According to our analysis, of the roughly 45 sites that were actively testing in San Antonio in mid-June, several sites with the lowest potential patient demand were concentrated in the northern neighborhoods of Stone Oak and The Dominion, as well as the areas surrounding Friedrich Wilderness Park, which are all majority-white communities that boast median household incomes ranging from around $100,000 to $150,000.
In comparison, many of the busiest sites are scattered in San Antonio’s more densely populated downtown, where the median income ranged from just $15,000 to about $40,000.
Throughout the San Antonio urbanized area, predominantly Hispanic neighborhoods had an average potential community need twice as large as white neighborhoods; the disparity in between majority-Black and majority-white neighborhoods was even larger.
Experts say that the disparity can be attributed to a longstanding gap in the health care system and an unequal distribution of health care facilities in the San Antonio area, which is one of the most economically segregated cities in the country.

Recognizing testing disparities in different communities, the city identified underserved neighborhoods based on its equity matrix, and put together three cost-free pop-up sites that rotate around different parts of the city every week, according to its health department.
Not only are government sites falling short of their ability to meet the public need for tests, but they themselves have become part of the disparity by concentrating demand even as they seek to address it in underserved neighborhoods. San Antonio’s walk-up sites do not require a doctor’s referral and, as a result, have become massively popular among those who do not otherwise have access to testing.
In late June, Jennifer Herriott, the deputy director of the San Antonio Metropolitan Health District, told us that people have lined up hours before these pop-up sites even open and that one time they had to turn down 275 people after running out of tests.
Herriott said that as the demand for testing spiked, with cases and hospitalization rates across the state setting new records on an almost daily basis, the city and the county have been working to ramp up testing capacity. The pop-up sites that used to run only three days a week now operate six days a week, and each site’s capacity has been increased from about 150-200 tests per day to 350.
Still, the long lines remain in some places, and sites continue to run out of tests.
“Public health and our partnership with San Antonio Fire [Department] has consistently had its eye on making sure that we're serving our black and brown communities,” Herriott said. “As our needs increase here, we've increased free testing and those walk-ups and the Freeman drive-thru so we make sure that communities that might not be able to access testing are able to access testing.”
Dallas
Dallas County and Tarrant County, two counties of nearly 4.7 million people that cover much of the Dallas urbanized area, have together reported nearly 64,000 confirmed cases of the coronavirus so far. Our data clearly showed that in early summer, the testing infrastructure of the Dallas urbanized area -- which encompasses the cities of Dallas, Fort Worth and Arlington -- resembled that of San Antonio: Local and state providers, as well as private hospitals, favored people living in whiter and wealthier parts of the county, towards the north, more than those living in the less affluent areas in the south.
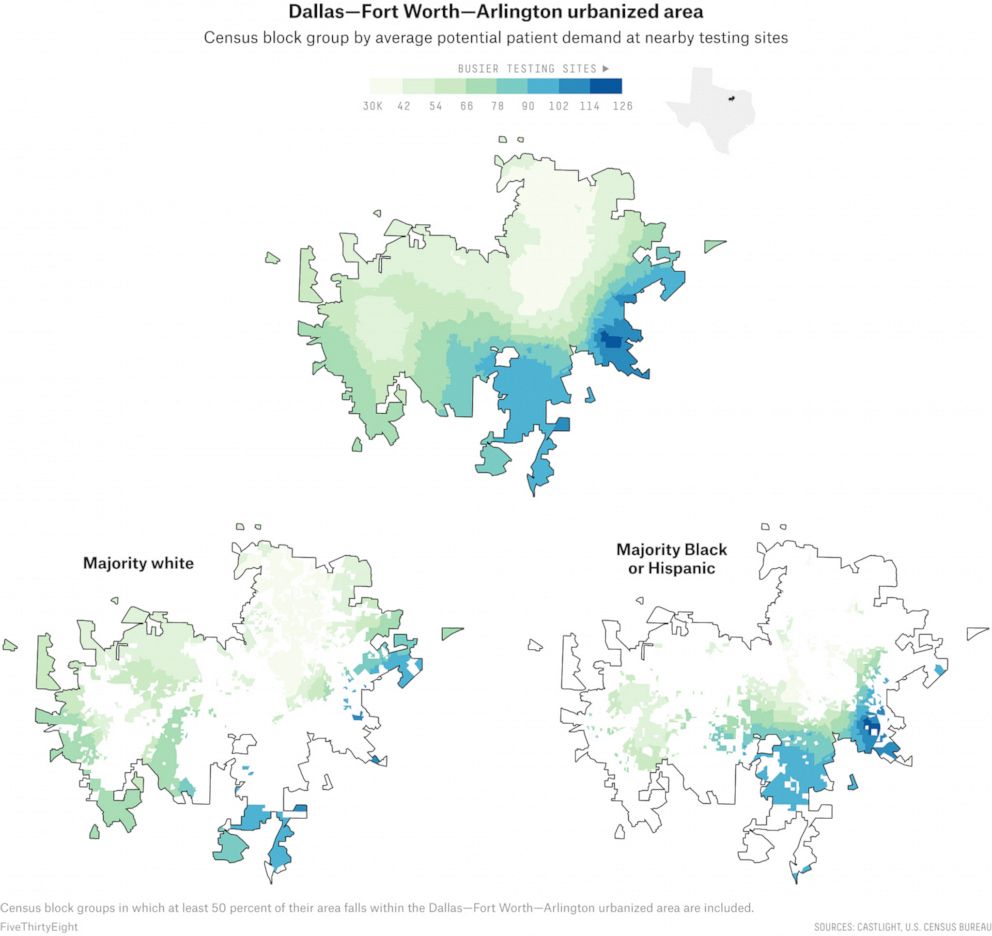
Across the Dallas–Fort Worth–Arlington urbanized area, our analysis found that majority-Black neighborhoods had a potential community need 71% higher than majority-white neighborhoods; majority-Hispanic neighborhoods had a potential need 44% higher.
“There’s a compounding problem beyond just where the sites are,” said Judge Clay Jenkins, the chief elected official in Dallas County. “The people that tend to have insurance are in the north and those that tend to not have insurance are in the south. We've planned to put the majority of our testing in places where there's high uninsured.”
Take the University Park neighborhood of Dallas, where the median household income is $214,000 and almost 90 percent of the residents are white. It has at least five testing sites around the neighborhood, according to Castlight data. Appointments are required at most of them, according to Castlight data, which helps organize the speed at which people are able to get tested every day (walk-in testing centers tend to have longer lines).
It’s a vastly different situation in Lancaster in southeast Dallas County, which has about 15,000 more residents than University Park but where Black people make up 69 percent of the population and the median household income is $53,000. Residents hoping to get a coronavirus test in the Lancaster area had to travel at least seven miles to the nearest drive-thru testing center until recently, when a nearby Walmart Supercenter opened up a drive-thru site.
To address the disparities, the city of Dallas asked the private sector to step up its support in the areas of the city most in need of more testing.
“A lot of the private providers are set up in northern Dallas, and it does highlight the existing disparities in the city,” said Tristan Hallman, a spokesman for Dallas Mayor Eric Johnson. “In response, we’ve asked Walgreens, CVS, Kroger to locate their facilities in southern Dallas, and they’ve done so.”

Indeed, public health experts said the issue of unequal access to testing is a direct result of longstanding decisions made by private-sector companies and entrepreneurs when deciding which neighborhoods to open new businesses in. And the disparity is exacerbated by the fact that underserved communities are less likely to have the health insurance or financial resources to seek costly testing from private providers when community sites are not accessible.
“This is certainly driven by systematic health care injustice and it’s actually very clearly delineated in Dallas because of gentrification and all of the social aspects of our community,” said Katelyn Jetelina, a professor at the UTHealth School of Public Health in Dallas. “We need to figure out how to supplement the cost so that families in south Dallas don’t have to decide whether they’re having dinner or have to go get a COVID test.”
Even as more testing sites have been set up in underserved communities, new coronavirus hot spots flared up over the summer as communities began to reopen; now, a lack of tests and long lines have created major problems all over the country.
Further south, along the border in Hidalgo, Texas, Isaac Garza waited 10 hours in line to get a coronavirus test after visiting several recently reopened restaurants he oversees. As he has diabetes, an underlying condition, he didn’t want to take any chances, and was relieved when his test results came back negative.
But the limited testing options in his community creates problems for Garza’s staff, too. Every day, Garza said, he receives calls from employees showing symptoms consistent with COVID-19 who tell him that they might have to miss critical work hours to wait in line for a test.
“It’s really been challenging to do business and just to live day in and day out with all this because you’re trying to protect your family, you're trying to protect your employees,” he said.
Laura Bronner is FiveThirtyEight's quantitative editor
Grace Manthey, a data journalist for ABC Owned Television Stations in Los Angeles, ABC News’ Briana Stewart and FiveThirtyEight’s Rachael Dottle contributed reporting.




