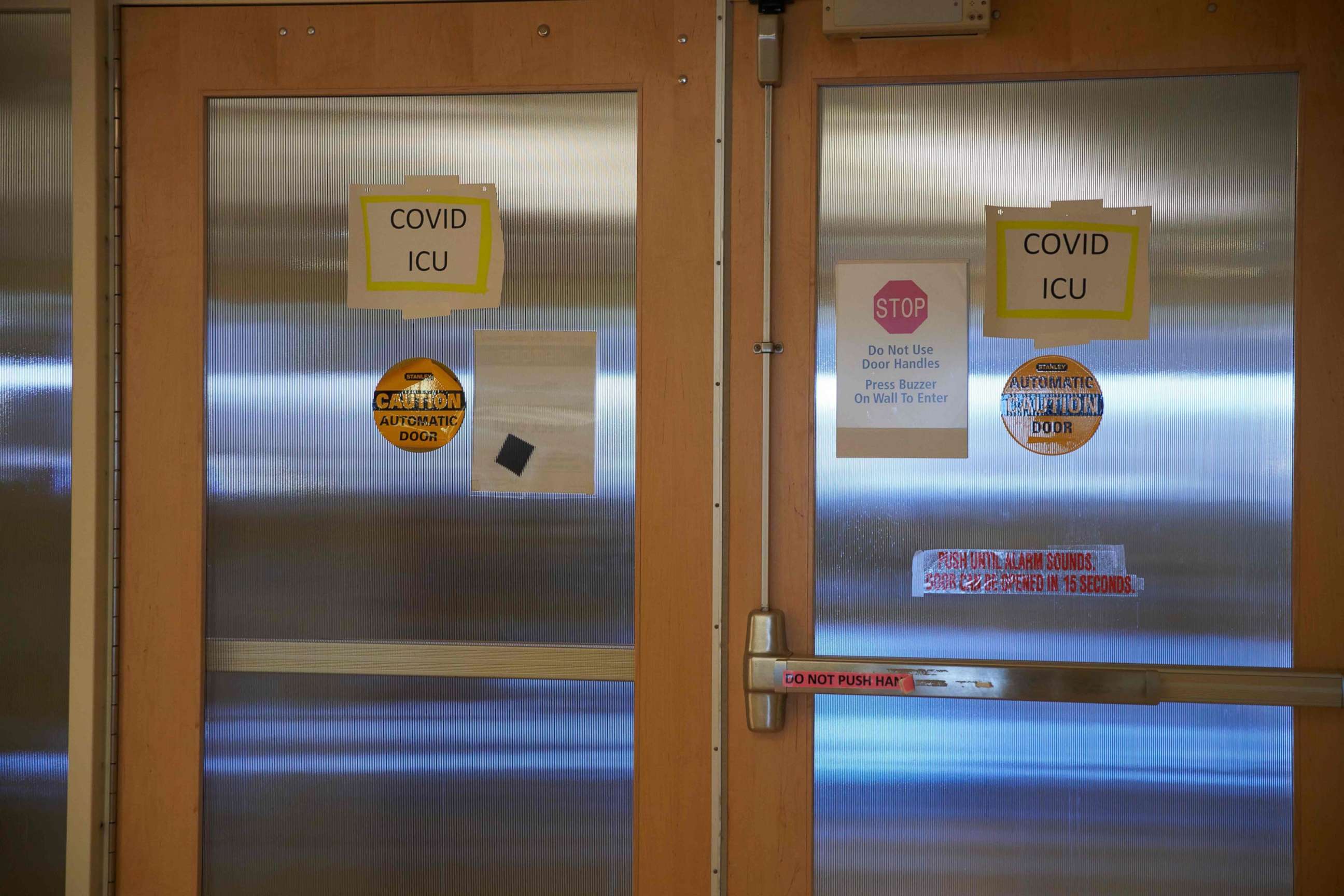
Hospitals struggle with space, staffing as COVID-19 cases skyrocket
More than 70% of ICU beds in the country's hospitals are full, HHS data says.
Hospitals around the country are facing shortages of hospital beds and intensive care unit space as the number of COVID-19 cases rise to record numbers, according to data released by the Department of Health and Human Services this week.
More than 76% of ICU beds in hospitals with the capacity to staff them are filled this week, according to an internal HHS memo obtained by ABC News.
HHS released new data this week providing even more detail on how hospitals are faring as COVID-19 case numbers continue to climb. The New York Times reported more than a third of Americans live in areas where hospitals have a critical shortage of ICU beds with more than 100 million Americans in regions where less than 15% of those beds were still available last week.

The dramatic increase in the number of Americans hospitalized for COVID-19 coincides with a shortage of hospital staff for about a fifth of hospitals in recent weeks, partly due to more health care workers contracting the virus outside of work.
Hospitals are facing increasing demand as the U.S. sees more than 200,000 new COVID-19 cases every day, according to data compiled by the COVID Tracking Project. That is three times higher than the peak of cases over the summer and more than six times higher than the peak in April. There are at least 104,600 people diagnosed with COVID-19 in hospitals around the country.
2.622 Americans deaths related to COVID-19 were reported on Tuesday.
And those numbers don't include the anticipated surge in cases associated with travel or gatherings over the Thanksgiving holiday. Dr. Anthony Fauci, one of the top infectious disease doctors in the country, says the holiday season will coincide with a very challenging period for the country.
"Given where we are right now coming off the Thanksgiving season, we have not yet seen the full blunt and and and the effect of the traveling and the congregating. That should be sometime probably next week, or a week and a half. Doctors, nurses, and public health officials around the country have been begging for their communities to comply with public health measures like wearing masks and avoiding indoor gatherings to reduce the pressure on the hospitals and staff that have been treating COVID-19 patients for months," Fauci said at a Wall Street Journal summit on Tuesday.
Independent advisers to the Food and Drug Administration are set to discuss emergency authorization for the COVID-19 vaccine developed by Pfizer this week but the limited supply of the vaccine won't have an impact on the widespread number of cases, so Fauci and other public officials say it's critically important to double down on protections such as wearing a mask, staying at home when possible, and avoiding indoor gatherings.
Andrew Carrol, an overnight hospital physician helping surge teams in Phoenix, said hospitals are seeing the same emergency cases that need intensive care treatment on top of COVID-19 patients. He said the hospital he's working in is "bursting at the seams" and trying to bring in personnel from out of state.
"We're running out of ICU beds. Now I don't mean just beds, we're running out of ICU teams, running out of those specialized personnel that helps take care of those people. So we're running out of capacity and so are a lot of other hospitals in Arizona," he told ABC News.
ABC News' Josh Margolin, Arielle Mitropolous, and Anne Flaherty contributed to this report.




