What to know about hepatitis A outbreaks in the US
The best defense against the disease is hand-washing and getting vaccinated.
Fears of hepatitis A swirled in Somerville, New Jersey, this week, after the health department there reported that a food handler in a local grocery store could have exposed shoppers to the infectious disease.
New Jersey's current hepatitis A outbreak, which began in 2018, has swelled to 504 cases as of early November.
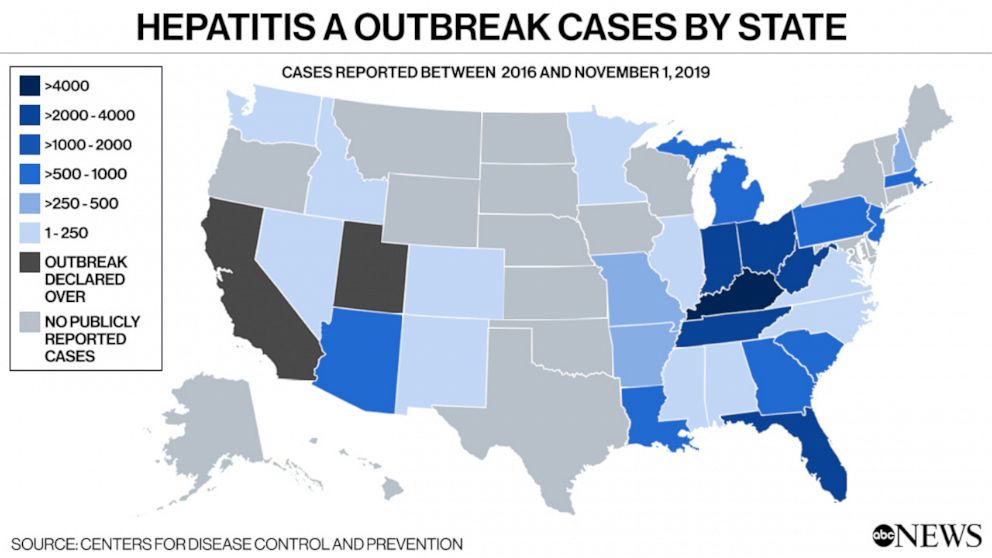
It's also part of an ongoing nationwide outbreak of the infectious disease, which began in 2016 and has led to 27,634 infections and 16,679 hospitalizations, according to the Centers for Disease Control and Prevention.
Hepatitis A, a highly contagious liver infection that's typically spread by coming in contact with feces from a person already infected, has killed 275 people in 30 states from 2016 through Nov. 1.
Despite the New Jersey grocery store incident, and contrary to what many people believe, most people don't contract the disease from contaminated food or water.
Instead, hepatitis A tends to be spread person-to-person, with the vast majority of infections occurring among people who are homeless or inject drugs, or among men who have sex with men.
California's 2016 to 2018 outbreak, for example, spread primarily among homeless encampments along the coastline, prompting then-Gov. Jerry Brown to declare a state of emergency.
Symptoms of the disease include fatigue, sudden nausea and vomiting, dark urine, clay-colored stool and jaundice, according to the Mayo Clinic. Unlike hepatitis B and hepatitis C, which also affect the liver, hepatitis A does not cause chronic liver disease, and is not typically fatal.
The best defense against the disease is thorough hand-washing and getting the hepatitis A vaccine, which is 95% effective and lasts for 11 years. Health experts recommend getting two doses of the vaccine, which provides at least 20 years of protection.




