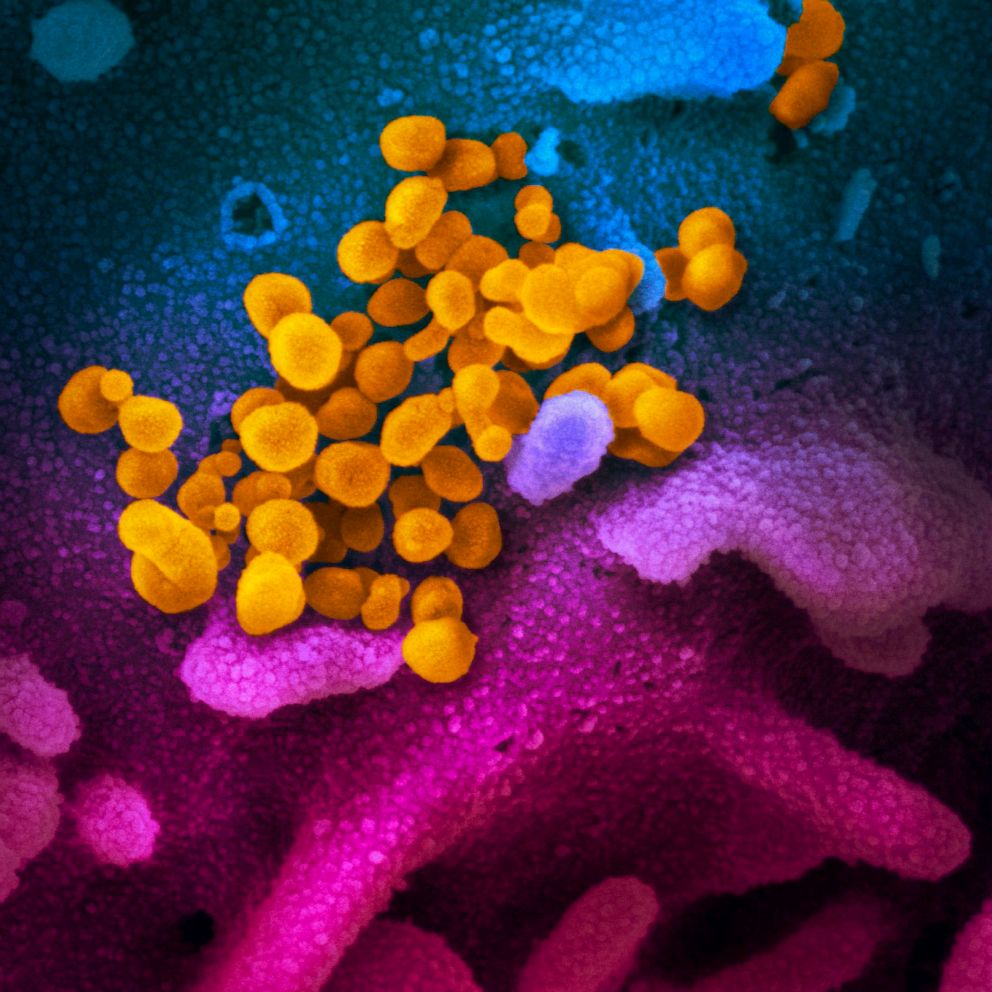
Coronavirus pandemic: How our preparation in the US now could shape our future
The estimated number of ICU beds in the nation is 46,500.
The World Health Organization declared last week that COVID-19 is a pandemic. At this time, experts do not know how wide the disease will spread, though prior estimates predicted that the worst-case scenario could be 60% of the world population being infected.
However, it should be noted that “being infected” is not the same as “being critically ill.” About 80% of patients will have only mild symptoms, with upper respiratory symptoms or mild pneumonia, according to estimates from the European Centre for Disease Prevention and Control.
Most of these cases can be handled by basic measures at home, including eating, staying hydrated, resting, and giving your body time to fight off the virus.
But the remaining 20% who do develop more severe illness will likely need to be hospitalized.
And with infections in the country quickly increasing, is the U.S. healthcare system prepared to handle this influx of patients?
Some experts have warned that if the United States experiences a sudden rush of patients, the healthcare system will be overwhelmed – akin to the way Italy’s resource-strapped doctors are now forced to make tough decisions about which patients to treat.
That’s why experts are emphasizing the importance of “flattening the curve,” which means taking measures now to prevent the disease burden from reaching a critical mass to overload a health system, through interventions suggested by the CDC, such as appropriate handwashing, covering coughs and sneezes, social isolation and quarantine.