Majority white counties have significantly fewer COVID-19 cases: Study
It's not about luck or genetics, experts said. It's structural racism.
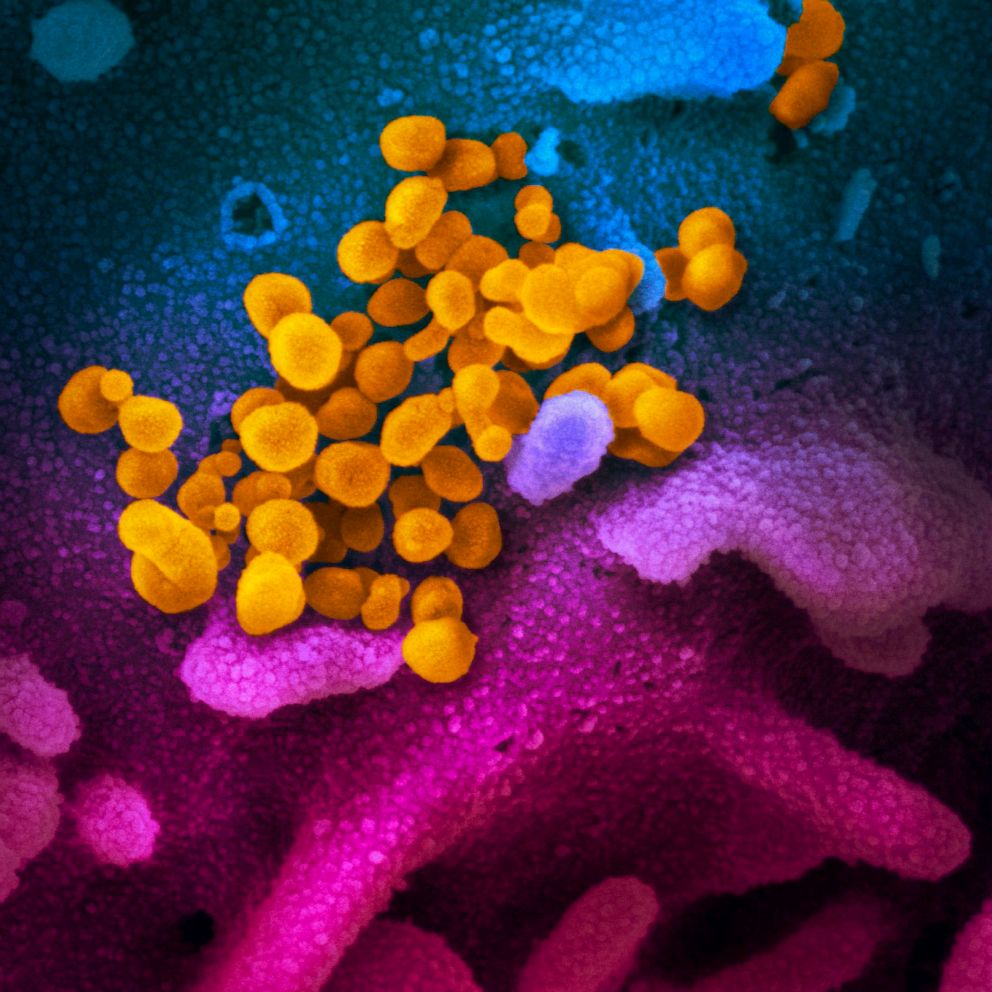
U.S. counties predominantly composed of white people have reported the fewest coronavirus cases, while diverse counties have been hit disproportionately harder by COVID-19, new research shows.
Researchers analyzed publicly available U.S. Census data and found that while 22% of counties have a predominantly Black population, those counties accounted for 47% of COVID-19 cases and 54% of deaths as of June. That racial disparity held true regardless of geographic region or political affiliation and was the same both before and after reopening the U.S. economy.
Counties that were more than 93% white reported the lowest rate of COVID-19 infections, at just 188 per 100,000 residents, compared with 914 per 100,000 residents in counties that were less than 60% white.
It's not that infections spread quickly in tightly packed cities and more slowly in spread out rural areas, according to the study, which was published in the journal AIDS Patient Care and STDs by the Foundation for AIDS Research. Instead, the disparities existed in every segment of American society.
"We found the same racial disparity among counties in small metropolitan and rural areas of the U.S.," the researchers wrote.
In addition to being more likely to get sick and die from COVID-19, Black and Hispanic Americans are more likely to have personal experience with a fatal COVID-19 case among friends, families and acquaintances. In a June survey, 31% of Black Americans said they knew someone who had died of coronavirus, compared with 17% of Hispanics and 9% of Whites, a Washington Post-Ipsos poll found.
"The premature reopening of our economy has only worsened the COVID-19 crisis among communities of color irrespective of region or blue or red voting patterns," the amfAR researchers noted.

COVID-19 disparities have roots in redlining, structural racism
Similar to many other Black-white health disparities, the researchers pointed to structural racism and residential segregation as key factors.
Crucially, neighborhood segregation isn't an accidental phenomenon, but rather an intentional outcome of historical systems like redlining, a policy that took root in the 1930s where lenders would refuse to approve loans for properties in largely minority neighborhoods.
The same structural racism that created those neighborhoods is a key mechanism in COVID-19 disease and death inequality rates. A similar analysis in New York City found that neighborhood quality affected HIV diagnoses, where 65% of Black men diagnosed with HIV in New York City and 68% of new HIV diagnoses among Black men were in high-poverty zip codes.
Similar to Black-white disparities in HIV rates, structural racism puts people of color at greater risk for COVID-19 infections, complications and death, the researchers found.
"Neither luck nor genetics keep COVID-19 diagnoses lower in mainly white counties and higher in primarily non-white counties," Greg Millett, amfAR's vice president and director of public policy said in a statement. "Adapting programmatic and policy interventions that have worked for HIV may help, but the historic legacy of residential segregation and redlining will have an enduring effect on health disparities until we decide to fix it."
What to know about the coronavirus:
- How it started and how to protect yourself: Coronavirus explained
- What to do if you have symptoms: Coronavirus symptoms
- Tracking the spread in the U.S. and worldwide: Coronavirus map
Tune into ABC at 1 p.m. ET and ABC News Live at 4 p.m. ET every weekday for special coverage of the novel coronavirus with the full ABC News team, including the latest news, context and analysis.