'The elephant in my room': How one doctor overcame the coronavirus
"My strategy changed by the day," Dr. Renee Eger said.
Dr. Renee R. Eger is an assistant professor of obstetrics and gynecology at Women & Infants Hospital in Providence, Rhode Island. Her views in this personal essay are her own and don’t reflect those of ABC News.
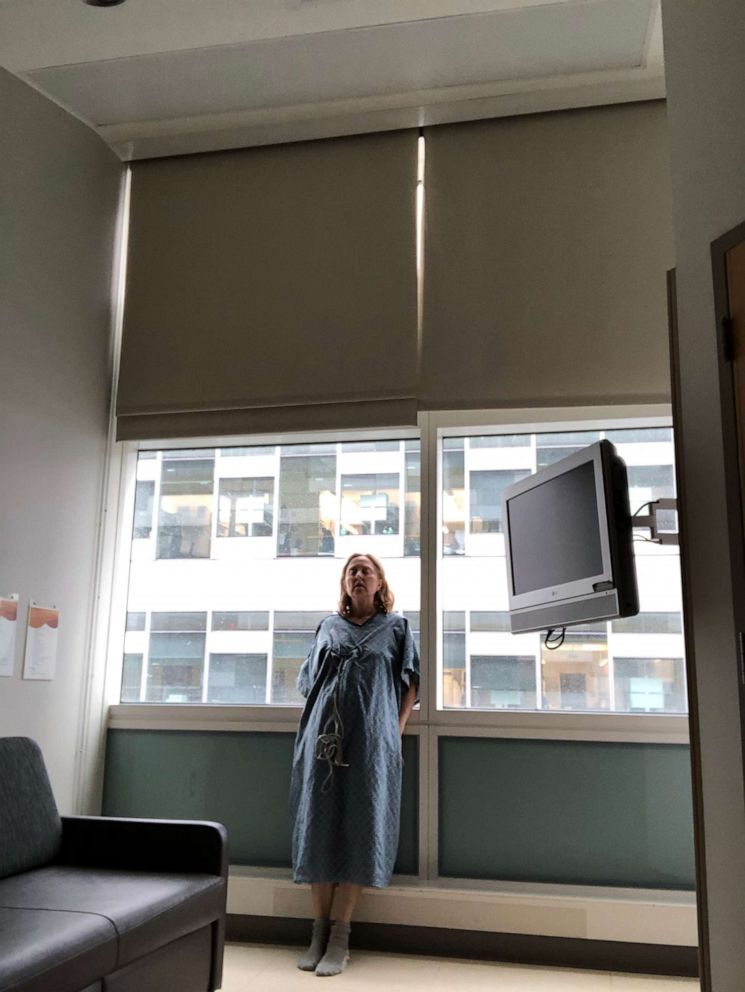
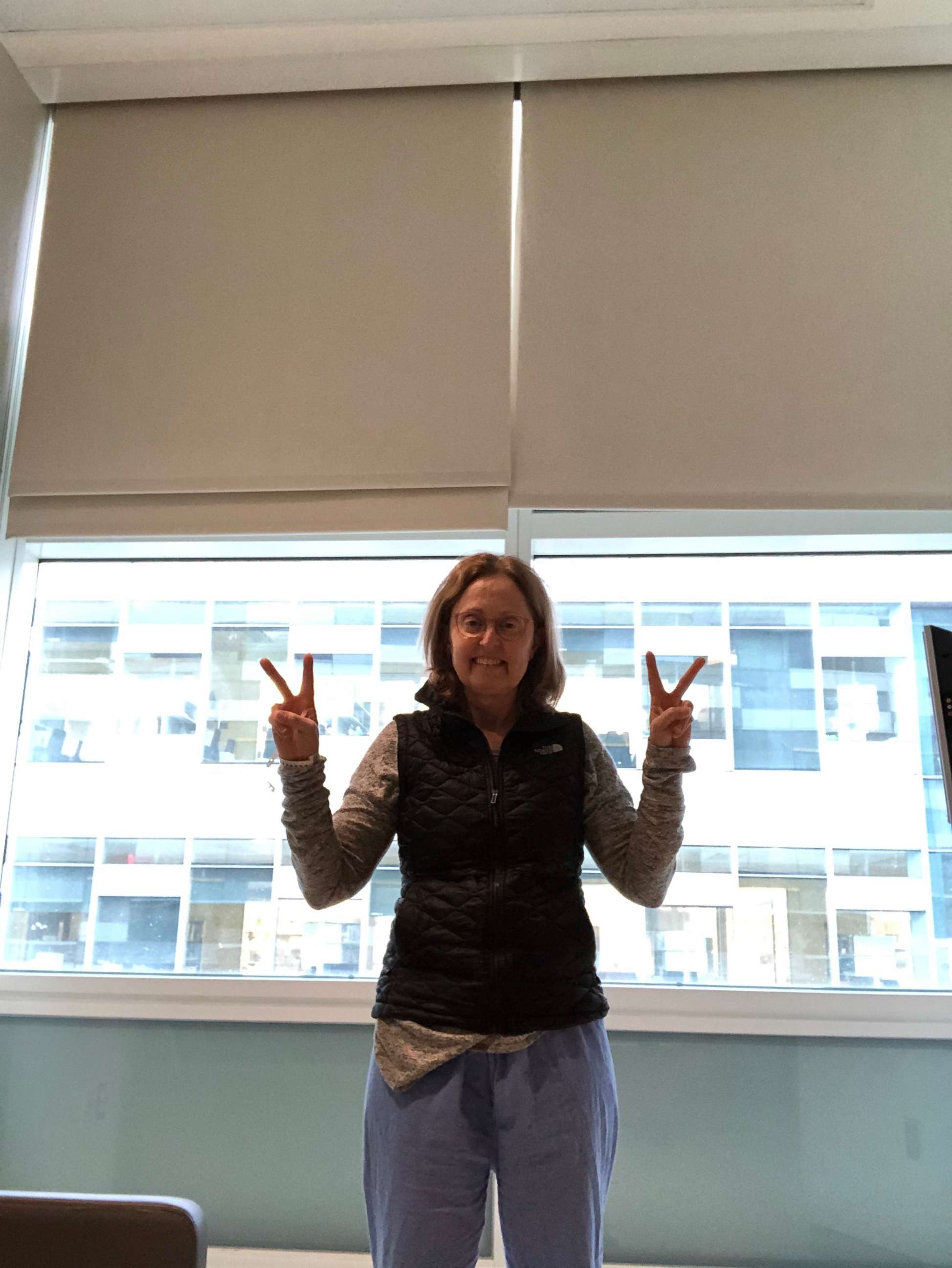
When I came down with COVID-19, I found my medical universe suddenly turned topsy-turvy and my only goal during the six days and nights that I spent at Brigham and Women’s Hospital in Boston was a modest one: to stay alive until Dr. Ebrahim Barkoudah’s next visit.
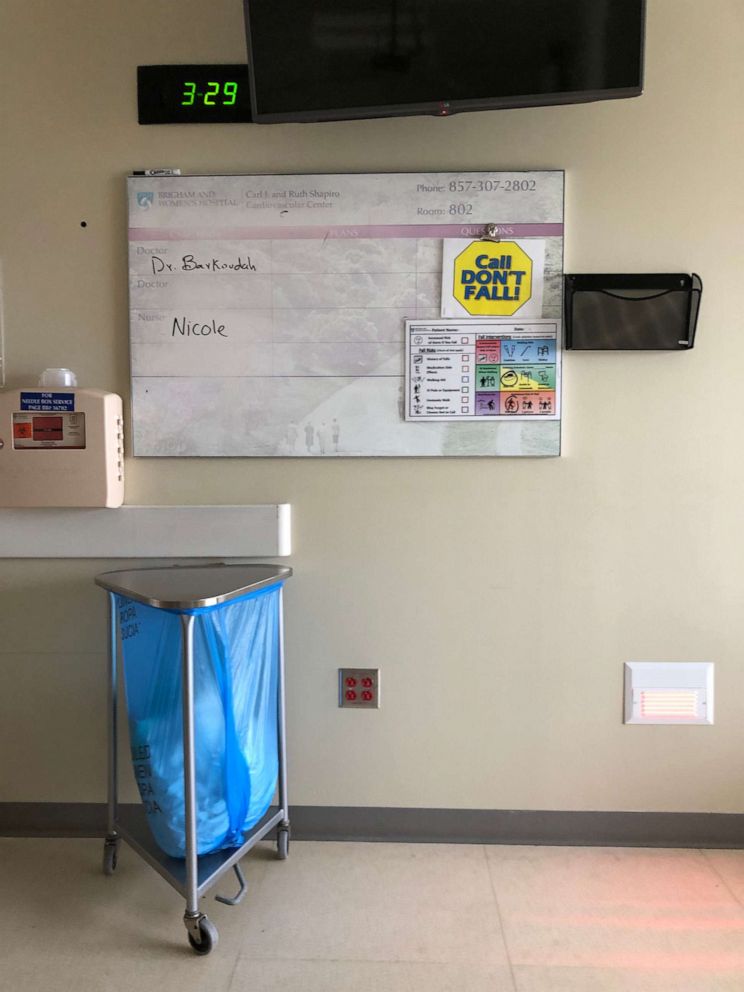
“You’re a member of our family now,” Barkoudah, the medical director at the hospital, said through his protective mask when he checked me in. His dark eyes smiled as he assured me I wasn’t going to die. “Our understanding of this disease is based on limited data. We are learning from you so that we can help you and others.”
Those were precisely the reassuring words I’d been offering young women in my 30 years as an obstetrician-gynecologist at Women & Infants Hospital in Providence, Rhode Island. Sometimes I'd believe what I was saying but I'd always know that hope was essential, no matter the actual odds.
It was on the seventh day of the war between COVID-19 and my gastrointestinal system when I found myself in an ambulance. I was febrile, short of breath and profoundly dehydrated from intractable diarrhea. I knew the probabilities.
The care I got was at once first-rate and rudimentary. No fancy drugs or special procedures; there are none for this novel plague.

All there is is Tylenol, a non-stop flow of intravenous fluids and whatever tenderness overstretched nurses could manage. Entering my room meant suiting up with a bouffant cap, N95 mask, face shield, plastic gown and gloves. Leaving meant discarding the gown and gloves in a biohazard box, waiting for a colleague to open the door and trying to shower away the unseen virus.
I was alone but I wasn’t lonely. Family, friends and coworkers were hanging on every word my physician husband wrote about my plight. People I hadn’t met were praying for me. But bearing witness to my own angst and fears took more energy than I had, so I didn’t. Not until now.
For all those days and nights, there was an elephant in my room. How was I going to beat this? What would it take? I’d heard the metaphor about the pitcher on the mound, nobody out, four runs in. He looks to the bullpen but it’s empty. In other words, any kind of relief would come from me alone.

My strategy changed by the day. First, I focused on making it to the bathroom and back. I disconnected my heart monitor and pulse oximeter, unplugged my IV pole, and dragged it behind me. I rested on the toilet, head between my knees, gathering strength for the return journey. My oxygen saturation dropped with each trip, a sign the virus had migrated to my lungs.
Spiking fevers were another one of my worries. I could take Tylenol every eight hours but I'd begin burning up long before that. I parsed time into two-minute intervals.
"10:36. Just make it to 10:38," I'd say, congratulating myself when the two minutes passed. "Those two minutes are done. Now make it to 10:40."
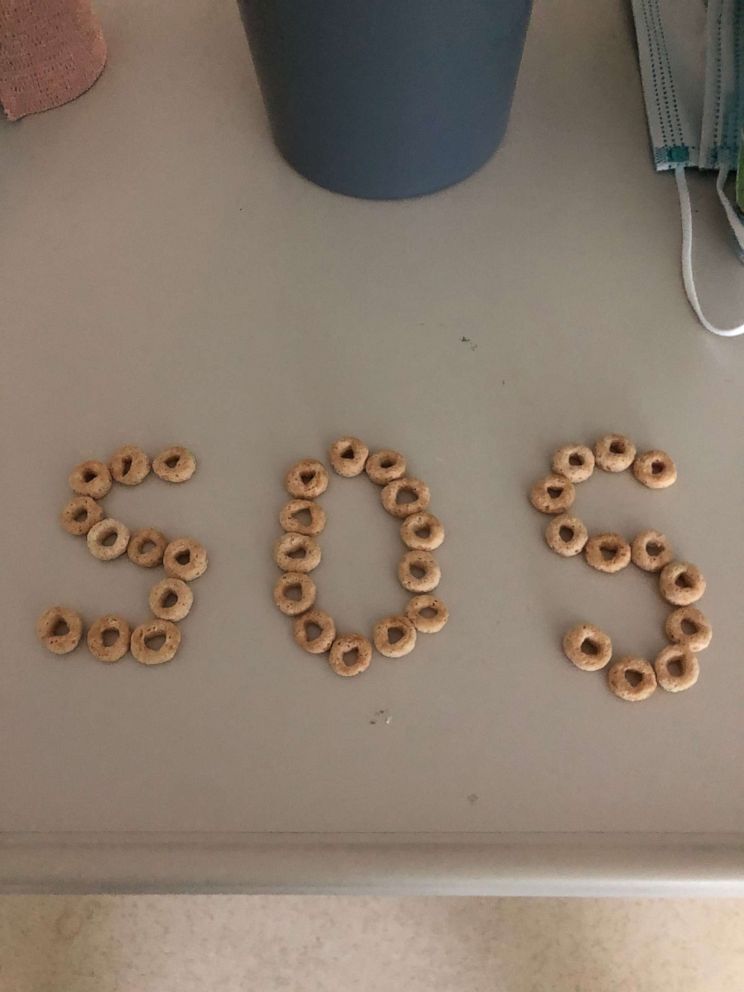
A tsunami roared through my gastrointestinal tract. My only nutrition came bathed in saline. I set daunting goals of 2,000 calories and 3,000 milliliters of fluid per day. Long gone was any sense of taste. When it returned, everything carried the smell of the virus. A bite of toast was like chomping into dry feces.
Breathing mattered most. As a doctor, I knew I needed an incentive spirometer, a handheld device used to improve lung function. But the few they had were for patients sicker than I was. So I jerry-rigged a system of dangling my legs over the bed, inhaling for a count of 15 seconds, then forcing the air out. Repeat. Repeat.

I knew an invisible team was caring for me. Food services sold its menu over the phone: “Get the Black and White Frappe. It’s our best seller!” Secretaries, aides and social workers offered support. But the only ones to enter my room were a nurse, physician or phlebotomist, one at a time.
The most heartening was Barkoudah, who would arrive at the end of each day, never leaving without the now ubiquitous era-of-the-coronavirus elbow bump and, in my eternally grateful case, helping me live to tell my story.
Renee R. Eger, M.D., medical director at the Obstetrics and Gynecology Care Center at Women & Infants Hospital and assistant professor and clinical educator at The Warren Alpert Medical School of Brown University




